Sciatic pain can sometimes be due to disc damage. But surgery isn’t always required. In this month’s case study, Dr. Detective meets a truck driver whose job-related stress gives him a literal pain in the butt – and fixes him with stretches rather than surgery.
Eat less and exercise more. It’s generally a great prescription for improving health and improving body composition. However, it doesn’t always work.
Even with an awesome exercise plan and a rock-solid diet, some people suffer from mysterious symptoms and complaints that seem puzzling, given how much effort they put into their fitness and health.
When we meet clients who have problems that exercise and nutrition — not to mention their own doctors — can’t seem to solve, we know there are only a few experts on the planet to turn to. One of them is Spencer Nadolsky.
Dr. Nadolsky is a doctor of osteopathic medicine who’s also studied exercise physiology and nutrition. An academic All-American wrestler in university, he’s still an avid exerciser and brilliant physician who practices what he preaches to patients -– treating preventable diseases first with lifestyle modifications (instead of prescription drugs).
When clients have nowhere else to turn, Dr. Nadolsky turns from a cheerful, sporty doctor into a meticulous, take-no-prisoners forensic physiologist. He pulls out his microscope, analyzes blood, saliva, urine, lifestyle – whatever he has to, in order to solve the medical mystery.
When Dr. Nadolsky volunteered to work on a regular case study feature with us, we jumped at the chance. By following along with these fascinating cases, you’ll see exactly how a talented practitioner thinks. You’ll also learn how to improve your own health.
In today’s case, we meet a man with sciatic pain who our doctor healed with stretches instead of surgery.

The client
55-year-old Ernest’s sciatica was getting worse.
One of my colleagues had seen Ernest about two weeks earlier and diagnosed him with lumbar radiculopathy. No, that doesn’t mean that Ernest was ridiculous. It means he had shooting pains down his leg.
“Lumbar radiculopathy” is what is called a symptom diagnosis. From the Latin radix, or root, and the Greek pathos, or disease, the fancy-sounding phrase just means, well, “shooting pains down your leg, probably originating in your lower back”.
Like other terms such as “arthritis” (“inflamed joints”) or sciatica (“Gee, your sciatic nerve sure is crabby”), this diagnosis just tells us what’s happening. It doesn’t actually explain why the patient hurts.
My colleague had sent Ernest for an x-ray to see if there were any structural abnormalities. Ernest was now back in my office to get the results. Oh — and also to tell me that his radiculopathy wasn’t any better. In fact, if anything, the pain was worse.

The client’s signs and symptoms
Ernest wasn’t in great shape, but he did care enough about his health to come for yearly physicals. He worked as a truck driver, which he said made it difficult for him to exercise. His job also influenced his diet. He ate a lot of fast food. Even so, he didn’t have too many medical problems… yet.
Although I had read my colleague’s note, as a good detective, I also wanted the history straight from Ernest. So we sat down and he repeated his story.
Over the past year or so, he explained, he had been suffering from a pain in the butt.
Or at least the pain began there. It then shot down to his right knee.
He’d never bothered to get it checked because he noticed it most when he was driving his truck. It would go away when he got out and moved around. So he figured it probably wasn’t anything very important. But recently, he was in pain more often than not. And it was really bothering him.
“Just cut to the chase, Doc!” he pleaded. “Tell me what’s going on! Will I need surgery?”
Ernest thought his x-ray would show some structural reason for his sciatic pain, like a herniated disc. But his x-ray was negative, which is very common in these cases.
This made it a job for Dr. Detective. I needed to perform another physical and ask Ernest a few more questions.
Messing around with neurological symptoms is no joke. As a doctor, you have to make sure you don’t miss something very serious like spinal cord compression from a tumor, or a serious spinal defect.
Luckily, Ernest hadn’t experienced any of the serious symptoms that typically come along with those, like urinary incontinence (wetting yourself) or saddle parasthesia (numbness between the legs). This was good news.
| Symptom | My thoughts – potential issues |
|---|---|
| Shooting pain from buttock to knee | Could be disc related, not likely tumor, no spine abnormalities on x-ray, maybe piriformis issues |
The tests and assessments
I was particularly interested in learning more about Ernest’s musculoskeletal system. He said he’d never had any surgeries or injuries. And of course I already knew that he sat in a truck all day. Ernest claimed he’d never had any unusual aches or pains in the past.
Visual assessment
I examined his shoes: worn-out Nikes. Hmmm. He also carried his big fat wallet in his right back pocket and said he did so regularly. Hmmm again. My detective’s nose was sniffing out clues.
Musculoskeletal assessment
Next up was a comprehensive osteopathic musculoskeletal exam. First I asked him to stand so I could check his alignment. Then I asked him to walk for a quick gait analysis. (Generally, physical therapists do a gait analysis with video, but this was a quick screening.)
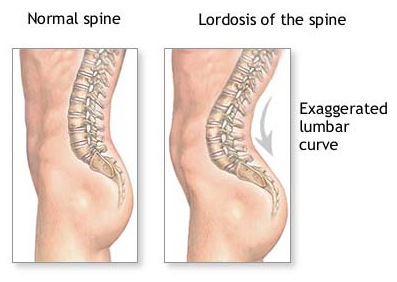
Ernest had the very common “Donald-Duck-butt” posture, or lordosis, with a forward-tipped pelvis. He swung his leg out a little bit as he walked. These might or might not have something to do with his pain.
 |
 |
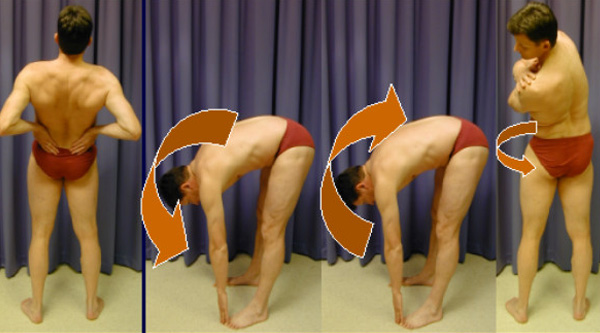
Since he was standing, I had him perform a standing flexion test to assess his innominate function (i.e. proper sacroiliac biomechanics). His test was positive on the right (in other words, the test revealed pain and dysfunction on the right side).
I put him face up on the table for the straight leg-raise test, which was negative. Folks suffering from disc issues that cause the pain down the leg sometimes test positive. This helped to rule out a disc problem in Ernest’s case – good news again. But it also deepened the mystery. If Ernest’s problem wasn’t a compressed disc putting pressure on the sciatic nerve, what the heck was it?
I checked his anterior iliac spine alignment, and then had him flip over to check his posterior iliac spine alignment. These were off.
And here’s where things got personal. I needed to palpate his piriformis.
In other words, I had to press on his butt cheeks.
That’s because I suspected that his piriformis – a flat, band-like muscle located deep in the buttocks, behind the gluteus maximus, and close to the sciatic nerve – might be the source of his discomfort.
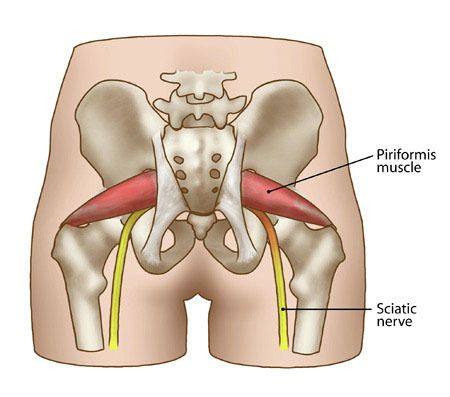
“Ouch!” Ernest cried out when I dug into his tender point. This was the pain he’d been talking about.
Bingo! It looked as if the pain was actually coming from the muscle.
Osteopathic alignment assessment
To address this pain, I’d need to align his innominates using muscle energy (an osteopathic stretching technique) and get his piriformis to relax.
I flipped Ernest back over so he was face up. (By now he must have felt like a pancake, with all this flipping.) I then performed a special hamstring stretch to his right leg.
First, with Ernest’s leg straight up, I found the “barrier” — the end of the stretch, where the leg would go no further. At this point, I asked Ernest to push his leg down against me for three seconds, then relax. This contract-relax cycle — known as proprioceptive neuromuscular facilitation, or PNF — uses the natural neurological response of the muscle to open up the range of motion.
I pushed his leg a little deeper into the stretch and the new, slightly further “barrier”. Contract-relax again. A little more range of motion. We repeated this sequence three times.

Finally, I checked his anterior iliac spines again.
Luckily, using this technique I was able to get his alignment close to normal. Misalignment might or might not be contributing to his piriformis problem, but it wouldn’t hurt to fix it.
Now back to the piriformis. I flipped Ernest back over onto his stomach and located the tender point on his right buttock again – much to his dismay.
I was about to perform what we osteopaths call “counterstrain technique.” I did this by keeping my finger on the tender point and moving his leg to the position that reduced the pain as much as possible, taking him from an 8/10 to a 3/10. I then held this position for about 90 seconds.
Ernest’s leg was now hanging off the table and flexed. When I brought him back up to his original position I rechecked the tenderness. Instead of measuring an 8/10 in tenderness and pain, he now reported that the pain was about a 4/10. This was an excellent result.
Dr. Detective to the rescue. Ernest was experiencing piriformis syndrome: His sciatic nerve was being irritated by the piriformis muscle.
The syndrome, which may or may not be recognized in regular Western medicine, is a pretty common sight in any osteopath’s practice. I told him we would take care of it for good and there wasn’t any reason at this point to get an MRI of his spine or to do expensive surgery.
The prescription
Ernest’s prescription was simple:
- Take the wallet out of his back pocket. A big fat wallet is a good problem to have, but keeping it in your back pocket (especially for years) can irritate your piriformis and sciatic nerve.
- Stretching and mobility exercises. I demonstrated the exercises Ernest should do at truck stops and at home whenever he got a chance, including a good piriformis stretch, which involved pulling his leg across his body. I opted against sending him to the physical therapist since his job limited his time and I wanted to see how he would do without extra guidance.
- Take some fish oil. I told Ernest it wouldn’t hurt to start taking some fish oil daily since it would probably help his overall inflammatory diet. I also said he could use some Tylenol if the pain got unbearable during the trip.
A sample piriformis stretch
Here’s an example of one of the simple stretches that Ernest could do — even while sitting in his truck.
While seated, cross one ankle over the opposite knee. Lean forward gently from the hips, keeping the spine straight. This stretches the piriformis of the top leg side (in this photo below, the right piriformis).

At-home self-massage
At Precision Nutrition, we’re big fans of foam rolling. You can do something similar to release the piriformis by using a tennis ball, lacrosse ball, or baseball under the hip. Just tuck the ball under your butt and roll around ’til you find the spot that makes you say unggghh.

The outcome
Ernest came back a month later. He’d taken my plan to heart and felt much better. Now he only felt pain when driving for very long periods. Needless to say, he was pretty happy.
Summary and recommendations
Sciatica can have many causes. It is important to diagnose the root cause correctly because some conditions are dangerous if left untreated. Luckily, Ernest’s problem was easy to fix — he had a different type of “trucker butt”.
- If you have sharp pain radiating from your lower back down your leg, get it checked out! The solution may be as easy as taking out your wallet and stretching, but it could also be a sign of something more serious that deserves medical attention.
- When you visit your health care provider, be sure to tell him or her about your daily routine and activities. Often, there’s a clue in there. Common culprits for sciatica include sitting a lot, driving, pressure on the hip joint (including sleeping on a hard mattress, such as a futon), and/or long-distance running or cycling.
- If your health care provider gives you a treatment plan, stick to it. Ernest was faithful with his stretches, which brought him almost immediate and dramatic relief. Rehab can be slow, but consistency pays off.
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.

Share