It’s a grim statistic: Most people who go on a diet and lose weight end up regaining that weight within a year.
Doesn’t sound too promising.
Why does this happen? Well, there are many reasons.
The big one is that people view a “diet” as a short-term solution and don’t really change their behaviours — which is why our Precision Nutrition Coaching program focuses on sustainable, permanent change.
Another reason is that our bodies have appetite- and weight-regulating hormonal mechanisms that try to maintain homeostasis (aka keep things the same) over the long haul. When we consistently take in less energy (in the form of food) than we expend through basal metabolism and activity (as in a diet or famine), our bodies respond by making us hungrier.
Our bodies don’t generally want to change. They like everything to stay the same. If we try to change things, our bodies will respond with compensation mechanisms, such as revving up our appetite hormones.
Two important hormones that shape our appetite and hunger signals are leptin and ghrelin. Let’s find out more about leptin, ghrelin, and weight loss.
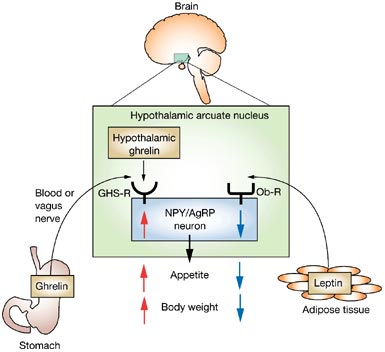
Hormonal control of appetite and body fat
Leptin and ghrelin seem to be the big players in regulating appetite, which consequently influences body weight/fat. When we get hungrier, we tend to eat more. When we eat more, obviously, we maintain our body weight or gain that weight back.
Both leptin and ghrelin are peripheral signals with central effects. In other words, they’re secreted in other parts of the body (peripheral) but affect our brain (central).
Leptin is secreted primarily in fat cells, as well as the stomach, heart, placenta, and skeletal muscle. Leptin decreases hunger.
Ghrelin is secreted primarily in the lining of the stomach. Ghrelin increases hunger.
Both hormones respond to how well-fed you are; leptin usually also correlates to fat mass — the more fat you have, the more leptin you produce. Both hormones activate your hypothalamus (a part of your brain about the size of an almond).
And here’s an important point: both hormones and their signals get messed up with obesity.
Leptin
Back in 1994, researchers noticed that one genetically altered strain of mouse ate a lot and was obese. When researchers administered a new substance, leptin (from leptos, or “thin” in Greek), the mice lost weight.
Soon after, nearly everybody interested in fat research was doing research on leptin.
At the time this was the holy grail of obesity research: a protein that made really, really fat mice into skinny mice. Fantastic! We’ll just make leptin pills, and everyone will be ripped, including the mice.
Well, like most things in biology, leptin is more complicated than that.
As it turns out, leptin injections only worked on mice (and people) who were genetically leptin deficient — only about 5-10% of obese subjects. The other 90-95% were out of luck.
How does leptin work?
Leptin is made by adipose tissue (aka fat) and is secreted into the circulatory system, where it travels to the hypothalamus. Leptin tells the hypothalamus that we have enough fat, so we can eat less or stop eating. Leptin may also increase metabolism, although there is conflicting research on this point. (1)
Generally, the more fat you have, the more leptin you make; the less food you’ll eat; and the higher your metabolic rate (possibly). Conversely, the less fat you have, the less leptin you have, and the hungrier you’ll be.
Basically, for weight loss — the more leptin the better.
Leptin resistance
You’d think, then, that fatter folks would somehow magically stop eating or start losing weight once their leptin levels were high enough. Unfortunately, you can become leptin resistant (2).
In that case, you can have a lot of fat making a lot of leptin, but it doesn’t work. The brain isn’t listening. No drop in appetite. No increased metabolism. Your brain might even think you’re starving, because as far as it’s concerned, there’s not enough leptin. So it makes you even hungrier.
It’s a vicious cycle.
- Eat more, gain body fat.
- More body fat means more leptin in fat cells.
- Too much fat means that proper leptin signalling is disrupted.
- The brain thinks you’re starving, which makes you want to eat more.
- You get fatter. And hungrier.
- You eat more. Gain more fat.
- And so on.
Leptin resistance is similar to insulin resistance (and they also share common signalling pathways). Insulin resistance occurs when there’s lots of insulin being produced (for example, with a diet high in sugar and simple carbohydrate), but the body and brain have stopped “listening” to insulin’s effects.
Interestingly, both types of resistance seem to occur together in obese people, though obese men who tend to have more internal belly fat (visceral fat) have higher insulin levels, and women who tend to have more fat under their skin have higher leptin levels (2).
Another leptin resistance fun fact is that fructose seems to induce leptin resistance (3).
There are a few possible explanations for how leptin resistance actually works. One theory is that leptin can’t get to the hypothalamus because the proteins that transport it across the blood brain barrier aren’t working or aren’t there, since there’s a buildup of leptin in the cerebral spinal fluid that bathes the brain (4).
Regardless of the actual mechanics, the important point here is that past a certain level, having more body fat can screw up your appetite signals and actually make you hungrier.
Ghrelin
Ghrelin was discovered 7 years after leptin, but after the leptin letdown, there was much less fanfare.
Leptin is a hormone that is a result of a buildup of fat, so it’s a long term regulator of body weight. Meanwhile, ghrelin is the short term Hey I’m hungry when do we eat? regulator.
Your stomach makes ghrelin when it’s empty. Just like leptin, ghrelin goes into the blood, crosses the blood-brain barrier, and ends up at your hypothalamus, where it tells you you’re hungry (1,5).
Ghrelin is high before you eat and low after you eat.
If you want to lose weight you want less ghrelin, so you don’t get hungry. If you want to gain weight, say if you’re scrawny, then you want more ghrelin — or at least you want it to stay high as you eat, so you’ll want to eat more.
Both hormones, as I mentioned, regulate appetite and hunger, and both of them regulate homeostasis — in this case, keeping you adequately fed. When you try to lose fat, your body will probably respond by changing hormone levels so that you get hungrier.
Obviously, this presents a challenge for folks trying to lose fat and keep it off — leading, perhaps, to the dreaded “yo-yo dieting” phenomenon.
Research question
Can leptin and ghrelin levels provide some explanation for the ups and downs that dieters experience? And could this relationship be more complicated than we expect?
This week’s review looks at how leptin and ghrelin levels are related to weight regain after dieting. (The title kind of gives the punch line away.)
Crujeiras AB, Goyenechea E, Abete I, Lage M, Carreira MC, Martínez JA, Casanueva FF. Weight regain after a diet-induced loss is predicted by higher baseline leptin and lower ghrelin plasma levels. J Clin Endocrinol Metab. 2010 Nov;95(11):5037-44. Epub 2010 Aug 18.
Methods
Researchers put over 160 obese and overweight men and women with an average BMI over 31.1 kg/m2 on a calorie restricted diet for 8 weeks.
This diet was 30% less (500-600 kcal/day) than the participants’ total energy expenditure, with 15% of calories from protein, 30% from fat and 55% from carbohydrates. There was no change in physical activity, just less food.
Researchers measured body weight, body fat and waist girths. They also took blood samples. Measures were taken before dieting (week 0), right after the dieting (week 8), and 6 months later (32 weeks).
Results
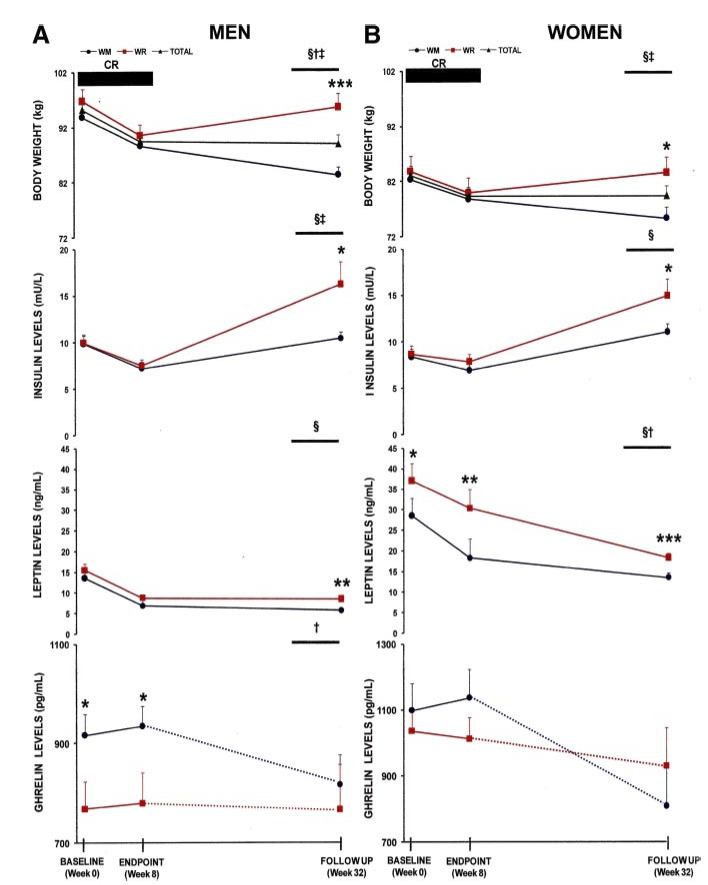
After 8 weeks on the diet, people lost an average of 5% body weight. Men lost 5.9% on average, and women lost 4.5%. They lost an average of 1.6% body fat and 4.1 cm off their waists.
Gainers and losers
But the average doesn’t give us the whole story. Some folks lost more than 5% of their weight, while others lost less. This may seem self-evident and not that interesting… until you look at their blood samples.
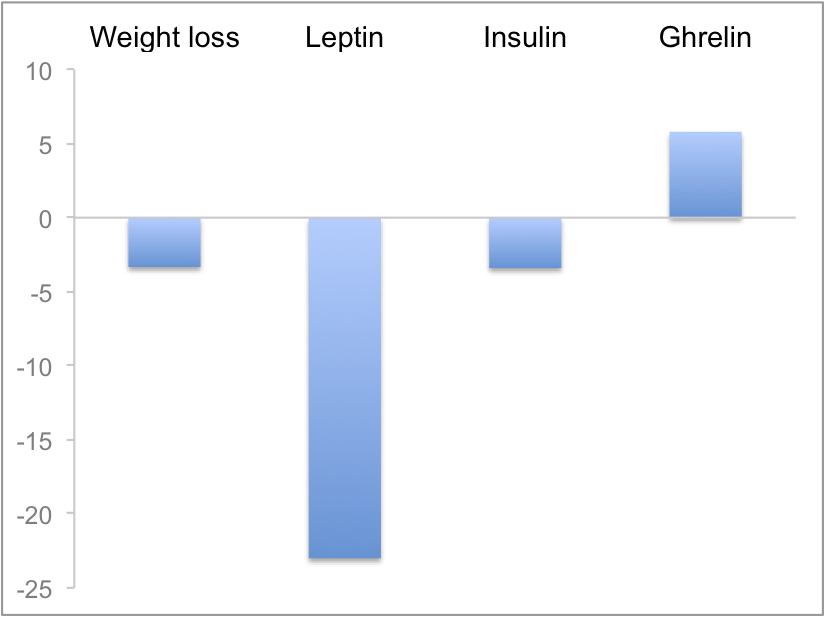
Dieters who lost more weight (>5%) had a bigger drop in leptin and insulin compared to dieters who lost less weight (<5%). Somehow losing weight is correlated to drops in leptin and insulin.
Figure 1 below compares the differences between the two groups. Compared to the <5% weight loss group, the >5% weight loss group:
- lost more weight (obviously)
- had lower leptin levels
- had lower insulin levels
- had higher ghrelin levels
This is pretty much what you’d expect.
Six month after the diet ended, this split continued. About half the group lost more weight; half the group re-gained the weight they lost.
Blood levels of leptin and ghrelin were correlated to weight loss or regain — and this effect often depended on sex.
- Women with lower blood leptin at the end of dieting were more likely to maintain their weight loss, but ghrelin didn’t seem to make a difference.
- Men with higher ghrelin levels at the end of dieting were more likely to regain weight, but leptin didn’t seem to matter.
- For both men and women, insulin levels at the end of dieting didn’t seem to matter in the long term, although insulin levels did increase when weight went back up.
- For both men and women, ghrelin levels were higher (meaning they were hungrier) at the end of dieting, but in weight losers, ghrelin levels dropped.
Huh.
Figure 2 shows the changes in hormone levels between weight maintainers (WM) and weight regainers (WR) at the start of the diet (0 weeks), end of the diet (8 weeks), and 6 months later (32 weeks). WRs are indicated by the red lines; WMs are the black lines with circles.
Discussion and conclusion
The biggest hurdle dieters face is weight regain — and dealing with it is a daunting prospect.
Appetite is controlled by a host of complex, interacting factors. This study suggests that the hormonal mechanisms may be different for men and women — and among men and women.
This difference may reflect the different hormonal environments in men and women. For instance:
- Ghrelin seems to be affected by growth hormone release, which differs in men and women.(6)
- Leptin seems to influence reproduction and fertility in women, which is related to women’s body fat levels. Women appear to be much more sensitive than men to leptin levels… unless men are given estrogen.(6)
- Intranasally administered insulin makes men less hungry and lose weight, but makes women hungrier and gain weight… unless women’s estrogen levels, or men’s testosterone levels, are low.(6)
However, there were also important differences within groups as well. Some men lost weight while others regained it. Some women lost weight while others regained it.
As the researchers point out, these findings suggest “the existence of two different populations according to the leptin and ghrelin levels [are] influencing the response outcomes”.
We’d expect that folks who regain weight easily would have lower leptin and higher ghrelin — making them hungrier. Not so in this study. The researchers propose that these results “are consistent with a disruption in the sensitivity to these hormone signals, probably in the central nervous system of those subjects with a higher predisposition to regain body weight.”
This suggests that in obese people, leptin and ghrelin signals may not always work in ways that we expect. Obesity can disrupt normal appetite signalling.
There is probably more to the story, and we’ll need more research to understand all the elements of weight loss.
Many factors in weight loss
Thus it appears that there are many important factors that shape successful weight loss.
If you’re looking for the silver bullet that will magically kill hunger and strip body fat off you, give up now.
Metabolic endocrinology appears to be only slightly more complicated than a nuclear reactor and brain surgery combined. No single hormone controls body composition, appetite, and hunger — and your individual hormonal profile may be relatively unique.
What’s also notable is that dieters who lost more weight on the diet had more significant changes in their appetite. They were probably hungrier while losing that weight.
Does the diet matter?
A few things that likely are contributing to weight regain are that this was a diet. Reduce calories for 8 weeks, lose the weight, then hope things work out for you. Obviously since it worked for some people, this method has some merit.
But as the data show, short-term diets alone don’t have a great success rate in the long run.
The macronutrient breakdown of this diet could also be relevant. It’s relatively low in protein, moderate in fat, and high in carbohydrate. We might see different hormonal effects with, say, a low-carb, high-fat, high-protein diet. (See last week’s Research Review on high-protein diets if you want to know more.)
What else can I do?
Strictly looking at improving ghrelin and leptin levels, some studies have shown that taking fish oil and getting regular sleep help. (7-9)
Other factors that help long term weight loss include:
- increased physical activity
- getting social support
- behaviour change techniques (e.g. goal-setting) (10).
Bottom line
Many interacting hormones shape our appetite and hunger. Several factors affect these hormones and our response to them.
So if you’re looking for a single solution — or rely on a short-term diet as a quick fix — you’ll probably be disappointed.
But there’s good news: There are many things that you can do that will lead to lasting body composition change.
- Take fish oil. Omega 3 fatty acids are linked to decreased hunger. (7)
- Sleep. Lack of sleep leads to more ghrelin and less leptin, as well as disrupted glucose and insulin metabolism. (8,9)
- Don’t get discouraged by these kinds of studies. Other research shows that it is possible to lose weight and keep it off — you just have to do a bit more than pop a leptin pill or do a few jumping jacks. The National Weight Control Registry tracks the features of successful losers. These include behaviour change, a commitment to good nutrition, and regular exercise.
- Understand that when losing fat, you might be hungrier. That’s normal.
- Enrol in the PN Coaching program. We’ve helped thousands of folks lose weight and keep it off for good. (And if you’re already in Lean Eating, congratulations! You’re well on your way!)
References
Click here to view the information sources referenced in this article.
Eat, move, and live…better.©
The health and fitness world can sometimes be a confusing place. But it doesn't have to be.
Let us help you make sense of it all with this free special report.
In it you'll learn the best eating, exercise, and lifestyle strategies – unique and personal – for you.

Share