Feed a cold and starve a fever, goes the old saying. But how should you consider eating when sick?
Nutrition expert Brian St. Pierre examines the evidence. He also shares some guidelines on what to eat, and what to avoid, next time you come down with a virus or infection.
- Want to see our visual guide? Check out the infographic here…
++
Remember the swine flu pandemic that pummelled North America in 2009?
I do. Because I had it.
I was down and out. Fever, chills, aches, pains, fatigue — the full catastrophe. I could barely move. Barely think.
The last thing I wanted to do was eat. Flaked out on the sofa for days on end, I dutifully drank my fluids and hoped for the best.
Eventually, like most otherwise healthy people, I recovered. My energy and appetite came back.
Afterwards, I wondered: Would tweaking my diet have helped me recuperate faster? Better yet: Could the right combination of nutrients have protected me from contracting the virus in the first place?
In this article, I’ll explore those questions and offer a few guidelines.
This way, next time you get sick, you’ll know exactly what to eat for a faster, smoother recovery. You’ll even learn how to reduce your chances of getting sick again.
The immune system: A primer
Intricate, complex, amazing: That’s the human immune system.
Standing guard throughout every part of our bodies, it protects us from the hordes of germs, fungi, and viruses that threaten to (literally) tear us apart.
In fact, when we eat, our immune systems get into the act from the very first moment we pop the food into our mouths.
Bet you didn’t know that your saliva contains powerful antimicrobials like lysozyme, alpha-amylase, and lactoferrin!
And these antimicrobials are only the basic, front line defense. Any germs that sneak past will confront a much more formidable barrier: our stomachs’ hydrochloric acid.
Corrosive enough to remove the rust from steel, hydrochloric acid will pulverize most invaders in our stomachs before they can reach our intestines.
If our stomach acids lose the battle, we also have proteins and chemical compounds further down the digestive chain that can sense and fight any harmful bacteria that may have made it past.
Finally, our own personal bacterial population (those probiotics you hear so much about) help prevent harmful bacteria from entering our bloodstream or taking root in our small intestine and colon.
The foods we eat affect these bacteria and the complex compounds they release.
Nutrient-dense, fiber-rich whole foods tend to promote a healthy bacterial balance, whereas a diet rich in processed foods, fats and sugars can lead to dysbiosis — otherwise known as microbial imbalance.
That’s why a balanced whole foods diet is your best insurance against all kinds of viruses and infections.
In fact, our GI tract comprises over 70% of our immune system! (And it’s a whole lot more complicated than we can go into here.)
For now, it’s enough to understand that what we eat affects immunity on many levels.
Keep reading to take a closer look.
Eating and immunity
If your diet is lousy, you’ll get sick more often than someone who eats a healthier diet.
Viruses and bacterial infections will hit you harder and keep you out for longer. Meanwhile, eating poorly while you are sick will only make you sicker.
Good nutrition allows our bodies to respond to germy invaders quickly and efficiently.
And in order to function well, the cells of our immune system need plenty of vitamins, minerals, amino acids, and essential fatty acids.
Yet nutrient deficiencies are far more common than you might suppose. That’s why at PN, we recommend you work to prevent them.
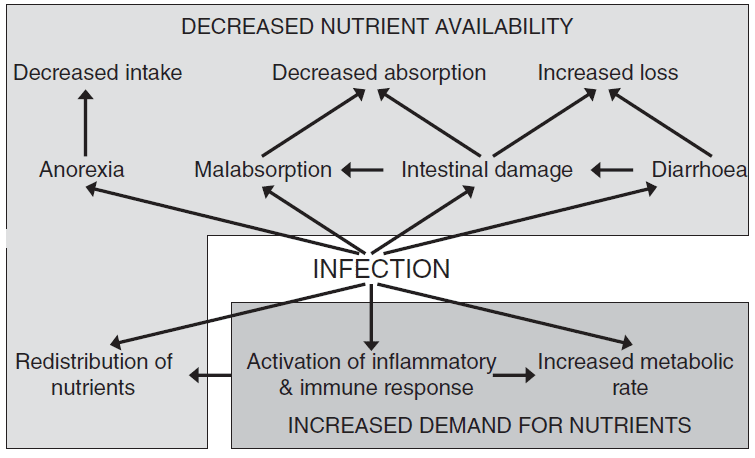
The opposing effects of infection on nutrient availability and demand.
(Calder PC. Feeding the immune system. Proc Nutr Soc 2013;72:299-309.)
Prebiotics and probiotics
Prebiotics and probiotics deserve special mention for helping to prevent illness. Both are essential to gut health. And gut health is essential to immunity.
Prebiotics (a.k.a. food for bacteria) help nourish our good microbial friends. Usually this is some form of semi-digestible fiber that our bacteria can chow down on, and/or that helps move food through the GI tract.
And probiotics (the bacteria themselves) have been shown to help us recover faster, once we get sick.
That’s why all of us should ensure that our systems are well colonized by these friendly critters.
The best whole food sources of prebiotics are:
- Vegetables: asparagus, garlic, Jerusalem artichokes, leeks, and onions
- Carbs: barley, beans, oats, quinoa, rye, wheat, potatoes, and yams
- Fruit: apples, bananas, berries, citrus, kiwi
- Fats: flax seeds and chia seeds
And the best whole food sources of probiotics are:
- Dairy: yogurt, cheese, and kefir with live and active cultures
- Fermented vegetables: pickles, sauerkraut, kimchi
- Fermented soy: miso, tempeh
- Miscellaneous: soy sauce, wine
Getting probiotics from food
If you’re healthy, aim for 1-2 servings of probiotic-rich foods each day. If you’re hoping to prevent or alleviate a medical problem, you may need to increase the dose.
Getting probiotics from supplements
Supplemental doses are typically expressed in billions of live organisms. Between 3 and 5 billion would be a starting dose. This could be increased to 10 billion if you are hoping to alleviate a specific health concern. Choose a reputable brand, and take it with food and water. See here for our recommendations.
Getting prebiotics from food
If you’re healthy, aim for 2-3 servings of prebiotic-rich foods each day.
Getting prebiotics from supplements
Taking 2-4 grams of prebiotics per day can help to feed healthy gut bacteria and keep things balanced. Supplementing pre- and probiotics at the same time might be a good idea.
Note: You may actually feel worse before you feel better, since bacteria release toxins. Ride it out for a few days and see what happens.
Also, immune-compromised people can develop infections from probiotic microbes. Be cautious if you:
- have AIDS,
- are taking immunosuppressive drugs,
- are receiving radiation or chemotherapy, and/or
- are in the hospital.
To eat or not to eat: That is the question
While a whole-foods diet rich in prebiotics and probiotics will go a long way towards protecting you from viruses and bacterial infections, even the healthiest diet can’t ward off every invader. And if you do get sick, of course you’ll want to recover faster.
Should you feed a cold and starve a fever, as the famous adage recommends?
Spoiler alert: There’s no definitive answer.
One small study did find that eating helps combat a cold virus. And fasting allows the body to fight fever-related infections.
But one study is far from conclusive. Especially when the reasons for its findings remain unclear.
What we do know is that moderate calorie restriction can:
- improve cell-mediated immunity and
- offset chemotherapy-induced and aging-related changes in immune function by helping to replenish stem cells.
On the other hand, during periods of very low food intake:
- our defenses against specific pathogens are lower, and
- the immune system is suppressed.
In the most severe cases, the malnutrition-infection cycle can ultimately lead to kwashiorkor (a severe type of malnutrition).
Sounds like a bit of a toss-up, doesn’t it?
Appetite and illness
With something to be said theoretically both for eating and fasting while sick, practically speaking, it’s best to rely on your own body’s signals.
In fact, when it comes right down to it, our own appetite cues probably give us the clearest picture of what we should eat (or avoid eating) when we get sick.
For example, very few of us want to eat when we’re hit by influenza or by gastroenteritis.
That’s because flu-like bugs and bacterial infections lead to higher levels of circulating TNF-alpha (an inflammatory cytokine), which promotes appetite suppression.
Maybe this is the body’s way of guarding its resources? After all, digestion takes a fair amount of energy — energy that may be better used to fight off invaders when we’re sick.
It’s an interesting possibility, but at this point it’s pure speculation.
The role of inflammation
We do know that behavioral and metabolic factors can influence immunity. Signalling mechanisms that control energy metabolism and immune function seem to be intertwined.
For example, our hunger hormone, ghrelin, may inhibit the creation of pro-inflammatory compounds.
And this can be a good thing or a bad thing — depending on circumstances.
How so? Well, inflammation helps us fight off invading pathogens. But too much inflammation will make our symptoms worse.
For example, a fever will increase metabolism as well as body temperature. This in turn improves the body’s chances of fighting off a bug — speeding it through the system.
At the same time, a fever can also dehydrate us, which makes it harder to move a pathogen through the body and out.
Meanwhile, infection itself can increase our body’s nutrient needs, especially for fluid, protein, and several micro- and trace nutrients.
Moreover, specific nutrients can affect immune function. A particular nutrient might be a source of fuel for an immune system cell, or it might influence other tissues that regulate overall immune function.
All in all, we’re talking about a very complex set of relationships. No wonder scientists have yet to get to the bottom of it all.
That said, considering that colds often result from viral infections, and fevers often result from bacterial infections, the advice to eat when you have a cold and fast when you have a fever does rest on some plausible biological arguments. Which is why, in cases of mild or moderate illness, it’s likely worth a try.
Especially if your own appetite agrees.
(Want to get the world’s most useful nutrition, health, and coaching strategies delivered straight to your inbox? Sign up for our FREE weekly newsletter, The Smartest Coach in the Room.)
Whole foods and immunity
Let’s say you get sick despite all your precautions — and your appetite doesn’t entirely disappear. Are there any particular foods that could hasten recovery?
As a matter of fact, there are.
A few examples:
- Garlic. Acts as an antibiotic, and has consistently been found to lessen the severity of colds and other infections.
- Chicken soup. Commonly touted as a food for colds, chicken soup actually works! It provides fluids and electrolytes, is warm and soothing, and may also contain anti-inflammatory properties that decrease cold symptoms. You have to use real chicken soup though — the kind you make from simmering a chicken carcass — rather than stuff from a can or package.
- Green tea. Boosts the production of B cell antibodies, helping us rid ourselves of invading pathogens.
- Honey. Has antibacterial and antimicrobial properties, and is an effective cough suppressant. In one study it was as effective as a cough-suppressing drug. A few teaspoons in a cup of green tea is all you need. (Plus, you’ll get the benefits of green tea at the same time.)
- Elderberries. These have antiviral properties and are loaded with phytonutrients. A few small studies have found the elderberry extract reduces the duration of colds and other upper respiratory tract infections.

Nutrients and immunity
Nutrition science loves studying isolated nutrients. At Precision Nutrition, that’s not really our thing.
We know that focusing too much on the details can sometimes lead people to forget the bigger picture — which is what most of us need to know in order to make healthy decisions.
Still, looking at specific nutrients can provide unique insight into metabolic pathways, and the effects of individual nutrients on specific circumstances. Plus, if you’re a science nerd, this is the kind of thing you probably enjoy.
A few examples of note:
- A major drop in energy can depress the immune system. This may explain why many people get sick a week or so after starting a crash diet.
- Inadequate or excessive intake of protein, iron, zinc, magnesium, manganese, selenium, copper, and vitamins A, C, D, E, B6, B12, and folic acid may all decrease the ability of the body to enlist immune defenses.
- Long-term nutrient deficiency, whether minerals, vitamins, protein, or calories, can reduce the immune system’s ability to respond. It’s a side effect of malnutrition and certain types of disordered eating. Actually, malnutrition was the leading cause of acquired immune deficiency before HIV. Adding a deficient nutrient back to the diet can restore immune function.
- Consistently over-eating, or eating more than the body needs, might also compromise how the immune system responds to invaders. Much of this might have to do with the fats we eat and ultimately store in the body. Dietary fats become part of cell membranes in the body, and thus influence how cells respond to invaders. Some fats seem to disrupt immune functions.
- While certain fats (like omega-3s) may help regulate immunity through resolvins and protectins, too many saturated, omega-6, or even omega-3 fats might sometimes be perceived as bacterial invaders and trigger an immune response, leading to a dysfunctional gut (and compromised immune system).
- Fat cells release inflammatory substances that can activate a “false alarm” immune response. Over time, the body gets tired of this false alarm and the immune system doesn’t respond as it normally would. This is similar to what might happen if you continually triggered your home smoke alarm by burning the toast — until finally you decided to take the battery out. When you actually have a fire, you’re screwed.
- Added sugars and high glycemic load diets may reduce white blood cell function and be pro-inflammatory. Gluten might also have a similar response in folks with a certain genotype.
- Dietary protein insufficiencies may lower immunity. At each meal, men should eat about two palms of protein dense foods, and women should eat about one palm.
- Iron and zinc are essential for various metalloenzymes necessary for nucleic acid synthesis and cell replication. Fancy words, but key components of healthy and well-functioning immune system. If these processes aren’t functioning properly, it’s tough for bone marrow to produce more white blood cells, and this in turn harms our immunity.
- Iron is a critical nutrient, but too much can lead to oxidative reactions that damage immunocompetent cells.
- Some have proposed that glutamine shortage may cause immunosuppression since glutamine is necessary for white blood cell proliferation. But data doesn’t prove this as yet.
Overall, both nutrient deficiencies and over-supplementation can actually diminish the body’s natural antioxidant defense system.
As always, balance is key.
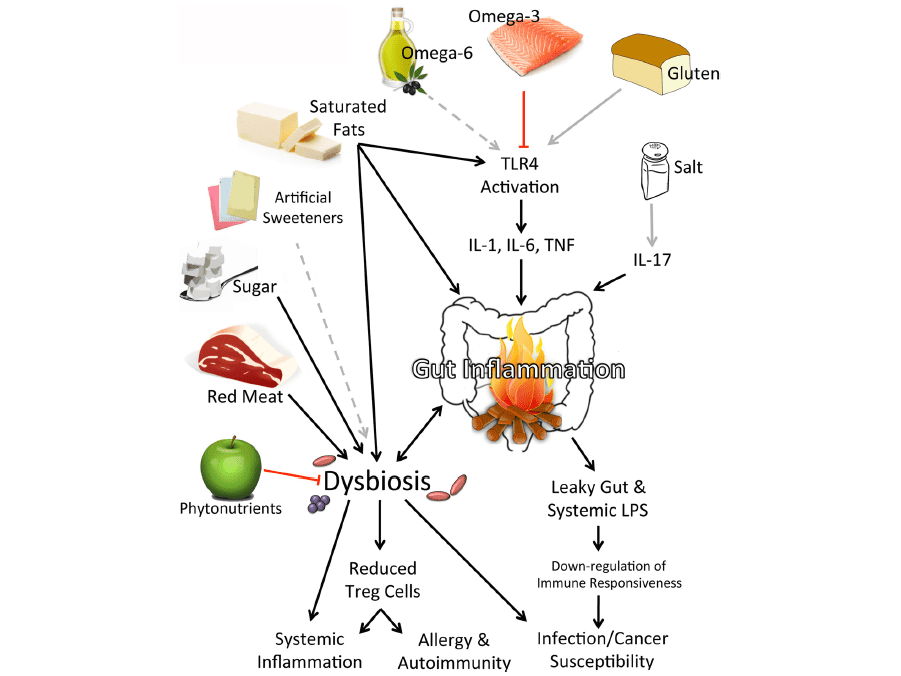
Components of the modern diet that might influence immunity.
(Myles IA. Fast food fever: Reviewing the impacts of the Western diet on immunity. Nutrition Journal 2014;13:61-78.)
Supplements
In general we use whole foods to improve our immunity. But under certain circumstances, you might want to supplement.
Nutrients that can support immunity and that are generally well tolerated include:
- Vitamin C supplements
- zinc
- elderberry extract
- ginseng
Quercetin may also assist in immune function (1,000 mg a day for 3 weeks). It’s found in onions, apples, red wine, broccoli, tea, and Gingko biloba.
Beta-glucan (found in oats) might help immunity.
Stevia might enhance white blood cell activity.
Selenium also appears to play a role in infection and changes in viral virulence (but be mindful of excessive supplementation).
Consuming foods rich in vitamin E (such as nuts, olive oil or avocadoes) may also help. This may enhance T cell function. And might lead to less influenza and fewer respiratory infections.
What you can do right now
To prevent getting sick:
- avoid over- or under-exercising
- avoid over- or under-eating
- maintain a healthy body weight
- wash your hands
- get enough sleep, consistently
- manage stress
- eat plenty of nutrient-dense foods
- feed your healthy bacteria
For some, periodic fasting might also be useful.
Also, consider supplementing vitamin D, probiotics, and a wide-spectrum food-based vitamin/mineral supplement.
But recognize that if you’re not eating a balanced, whole food diet, supplementing with probiotics won’t do a lot of good. An isolated supplement can’t fix a broken diet. Address your diet first.
If you’re already feeling sick:
- drink lots of fluids (especially water and green tea)
- rest and recover
- focus on immune-boosting foods
- supplement with pre- and probiotics
- use immune-boosting supplements
And above all, listen to your body cues.
If you’re hungry, eat. If not, don’t. Either way, Super Shakes may come in handy.
In the end, no matter how well you manage your nutrition, exercise, sleep, and stress, you will get sick sometimes. We all do.
Don’t be a hero and pretend you’re not. Instead, take the steps outlined here to get back on your feet as quickly as possible.
(Also see our comprehensive article on Exercising when you’re sick: Sweat it out? Or rest and recover?)
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We'll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)

Share