Basics | IgG Tests | Free Tests | Accuracy | Downsides of IgG Tests | Meal Planning
Do expensive food sensitivity tests work?
Are there lower cost (or free) ways to root out food sensitivities?
And, perhaps most important, what should people do with their results?
In this article, you’ll learn the answers to those questions (and more!), including:
- The different types of food sensitivity and allergy tests—along with which ones work and which ones don’t.
- 3 often-overlooked problems with IgG food sensitivity tests.
- Surprising issues that mimic food sensitivities.
- Strategies nutrition coaches can use to talk to clients about food sensitivity testing.
- A simple, FREE tool that will help you quickly and easily plan delicious meals, regardless of how many foods appear on your “don’t eat” list.
+++
Why get a food sensitivity test?
When people decide to get a food sensitivity test, they’re usually desperate to feel better. For years they’ve been bothered by stomach upset, bloating, embarrassing gas or belching, abdominal pain, diarrhea, and/or brain fog.
Despite giving up any number of foods—gluten, dairy, onions, garlic, this list goes on—their problems persist.
So, when they learn about food sensitivity tests that require only a finger prick’s worth of blood, they’re relieved. They can’t wait to find out what’s wrong—and finally get back to living without an unpleasant digestive emergency lurking around the corner.
How do I know this?
As a registered dietitian, I’ve counseled hundreds of people with mysterious and maddening GI woes.
Plus, I was practically born with an upset stomach.
During my childhood, my mom took me from one specialist to another. Medical experts suggested I might be sensitive to gluten. Or maybe dairy.
Or gluten and dairy?
No matter what I stopped eating, I just couldn’t shake my digestive issues.
By the end of high school, I had the runs nearly every day.
If you can imagine that, then you can no doubt understand why I decided to major in nutrition and eventually become a registered dietitian. I was looking for answers to help me solve the problem once and for all.
Maybe you can also understand why, during my freshman year in college, I found myself in the waiting room of a naturopathic physician who offered food sensitivity testing.
Despite what the test revealed that day, it would take me years to unravel what was really wrong. And that long search taught me many important lessons.
The best ways to identify and deal with food sensitivities.
Most people can test for food sensitivities and intolerances at home—no needles, blood work, or special kits required.
Though at-home options like food journaling and elimination diets aren’t as easy as pricking your finger and sending your blood off to a lab, they’re more accurate and effective.
And there’s this: Some people—myself included—can clear up their symptoms without giving up a single food.
Put another way, millions of people are convinced that they can’t eat dozens of foods when, in reality, few (and, in some cases, none) of those foods are actually a problem for them.
I’ll explore all of that in this article, diving deep into the latest science as well as my personal experiences.
It’s my hope that what you’re about to learn not only helps you understand what’s actually going on, but also allows you to enjoy eating a wide variety of foods again, without fear. (Related: ‘What foods should I eat?’ Your three-step guide to choosing the best foods for your body.)
Let’s start with a few definitions.
What are food sensitivities?
Some people use the term “food sensitivities” as a catchall to describe a wide range of adverse symptoms that can be brought on by eating certain foods.1
Other people define sensitivities more narrowly.2 For them, food sensitivities are what’s left over when the following problems are ruled out
- Food allergies: When the immune system mistakenly treats a component in food as if it were a germ. This can lead to a wide range of allergic responses: hives, swelling, vomiting, diarrhea, and life-threatening drops in blood pressure.
- Food intolerances: The inability to process or digest certain foods. For example, someone who is lactose intolerant doesn’t have adequate amounts of the digestive enzymes needed to break down lactose, a sugar present in dairy products.
- Celiac disease: An autoimmune reaction that triggers gut inflammation and diarrhea when someone consumes gluten, a protein found in many grains, most notably wheat.
Still other people use the word “sensitivity” interchangeably with “intolerance.” They throw around the term IBS (short for irritable bowel syndrome)—trying to indicate that something in the diet is making someone feel sick, but they’re unsure of the culprit.
It’s all pretty confusing, so let’s make it simple.
For the purposes of this story, I’ll borrow a definition from the American Academy of Allergy Asthma & Immunology: “A food sensitivity occurs when a person has difficulty digesting a particular food.”3
Types of food sensitivity tests: What works?
Alrighty, so let’s circle back to what I started to tell you at the beginning of this article—about the day I underwent food sensitivity testing.
The naturopath pricked my finger and sent a few drops of my blood off to a lab.
About a week later, the doctor handed me a 10-page report that, she said, revealed I had a “weakened” immune response to dozens of foods: sugar, dairy, cooking oil, gelatin, baking powder, cornstarch, chocolate, butter, cheese, popcorn, pretty much all grains, veal, liver, beef, tree nuts, corn, Brussels sprouts, and cabbage.
As I glanced over the report, I considered the food typically served at the campus dining hall.
I’d wanted clear answers and a workable plan to put into action. Instead, I left feeling overwhelmed and helpless. How could I possibly eliminate all of those foods for the rest of my life?
Is IgG food sensitivity testing accurate?
With food sensitivity testing, a lab analyzes how immunoglobulin G (IgG), an immune system antibody, reacts to roughly 100 different foods. The idea is that elevated IgG levels signal a food sensitivity.
This premise seems logical.
After all, that’s similar to the premise of food allergy blood testing, which measures a different antibody called Immunoglobulin E (IgE).
When levels of IgE are elevated, it indicates someone’s immune system is pumping out substances that trigger parts of the body to swell up, break out in a rash, shut down, and/or eject things from the GI tract (a.k.a. vomiting).
Though IgE tests can deliver false positives, they’re relatively accurate, correctly diagnosing allergies 70 to 90 percent of the time.4 This is how you can know if you have, say, a nut allergy.
Unlike IgE tests, IgG tests are unregulated and unproven.
The few studies that seem to support IgG testing have been criticized for a variety of design flaws.5
(To learn what to look for in a study, see How to read scientific research.)
The premise behind IgG tests has also been called into question. That’s because elevated IgG probably isn’t a bad thing. Most experts consider it a normal immune response.
Our bodies likely develop IgG antibodies to all the foods we eat.
These antibodies may even be how the body marks a substance as “safe.”
As the chart below shows, when IgE is high, someone likely has a food allergy. But when IgE is low and IgG is high, it’s a sign that the body has become tolerant to a particular food.6
| IgE | IgG | |
|---|---|---|
| Likely food allergy | High | Low |
| Likely food tolerance | Low | High |
Put another way, if your blood reacts with IgG to a specific food, it probably doesn’t mean you’re sensitive to it. Rather, it may mean you’ve eaten that food somewhat recently.5,7
As a result the following organizations all strongly recommend against taking IgG food sensitivity tests:
- American Academy of Allergy, Asthma & Immunology3
- The Canadian Society of Allergy and Clinical Immunology8
- The European Academy of Allergy and Clinical Immunology7
As the Canadian Society of Allergy and Clinical Immunology put it:
“The inappropriate use of this [IgG food sensitivity] test only increases the likelihood of false diagnoses being made, resulting in unnecessary dietary restrictions and decreased quality of life.”
3 big downsides of IgG tests
Maybe you’re thinking: So what if IgG tests are unproven? Does it really matter if someone wastes money on a test that doesn’t work?
It does matter—for at least three important reasons. An inaccurate food sensitivity blood test may mean that:
- You continue to eat foods that could be the source of your issues—because those foods didn’t react to the IgG in your blood.
- You stop eating a lot of foods that are perfectly okay for you to eat. That’s no fun. Worse, you could develop nutrient deficiencies.
- You fail to diagnose the true problem. This was the case with me. Roughly fifteen years after my IgG test, I underwent a colonoscopy. It revealed a rare, incredibly slow-moving, genetic ovarian tumor—one I’d likely had since birth. The tumor had grown outside of my ovary and through the wall of my digestive tract. Once I had my cancer removed, my digestive problems vanished.
Important note: All three of these downsides—especially the risk of nutritional deficiencies—intensify when children are involved.
On top of the drawbacks listed above, when young children are coddled and prevented from exposure to various foods, they’re more likely to develop allergies and/or sensitivities to those very foods as they get older.9
All this begs the question: How can you find out whether you really have food sensitivities? And if you do, what should you do about them?
6 problems that mimic food sensitivities
I thought I had food sensitivities. In reality, I had cancer—a tumor that had invaded my digestive tract.
My situation, however, is incredibly rare. Most people with bloating and frequent diarrhea don’t have cancer. Much more common, however, are the following:
1. A tendency to gulp down dinner
When we eat quickly, we swallow air bubbles, which lead to a puffy, bloated, gassy feeling.
And because it takes some time for the “I’m full” signal from the stomach and intestines to reach the brain, fast eating often triggers overeating, which only compounds that uncomfortable post-meal sense of unease.
(If you want a strategy that could be helpful here, check out the 30-day slow eating challenge.)
2. Too much fiber too quickly
Some people experience stomach pain, gas, and bloating after suddenly increasing their fiber intake.
For example, a client might decide to start eating nine servings of vegetables for a New Year’s resolution. If they hadn’t eaten many veggies before, this sudden change will overwork the GI tract’s peristalsis muscles as well as disturb the flora that live in the gut.
When they temporarily reduce their fiber intake and then slowly increase it, they feel a lot better.
3. Not enough fluids
Water is also incredibly important, as it helps to move stool through the digestive tract. Getting enough becomes essential if someone is increasing fiber intake.
A good general rule: When adding a serving or two of fiber, up your water consumption by 1-2 glasses.
4. Gut flora imbalance
Antibiotics can wipe out levels of friendly gut bacteria, allowing more problematic bugs to take over, leading to diarrhea and other symptoms.
Starting Lactobacillus rhamnosus GG (for children) or Saccharomyces boulardii (for adults) within two days of your first antibiotic dose may help reduce the risk of antibiotic-associated diarrhea.10
5. Stress and lack of sleep
Stress diverts blood flow away from the GI tract, making it harder for the body to digest food effectively. End result: gas, pain, and bloating.
Before meals, I encourage my clients to try a Box Breathing sequence:
- Inhale for 4 seconds.
- Hold for 4 seconds.
- Exhale for 4 seconds.
- Hold for 4 seconds.
- Repeat 3 to 5 times.
This short breathing exercise helps trigger relaxation, sending blood flow to the GI tract, priming it to digest the food about to be eaten. It can also help people to slow down.
End result: the heartburn, stomachaches, and bloating eases.
(For more strategies on how to reduce stress, read: How stress prevents weight loss.)
6. Food aversion
Sometimes the mere thought of a food may make someone sick, though the mechanism isn’t fully understood.
These aversions often occur in young children who’ve gotten sick—for example, from food poisoning or stomach flu—after eating a particular food. Their brain then seems to link the nauseated sensation to the food.
Zero-cost ways to test for food sensitivities—at home
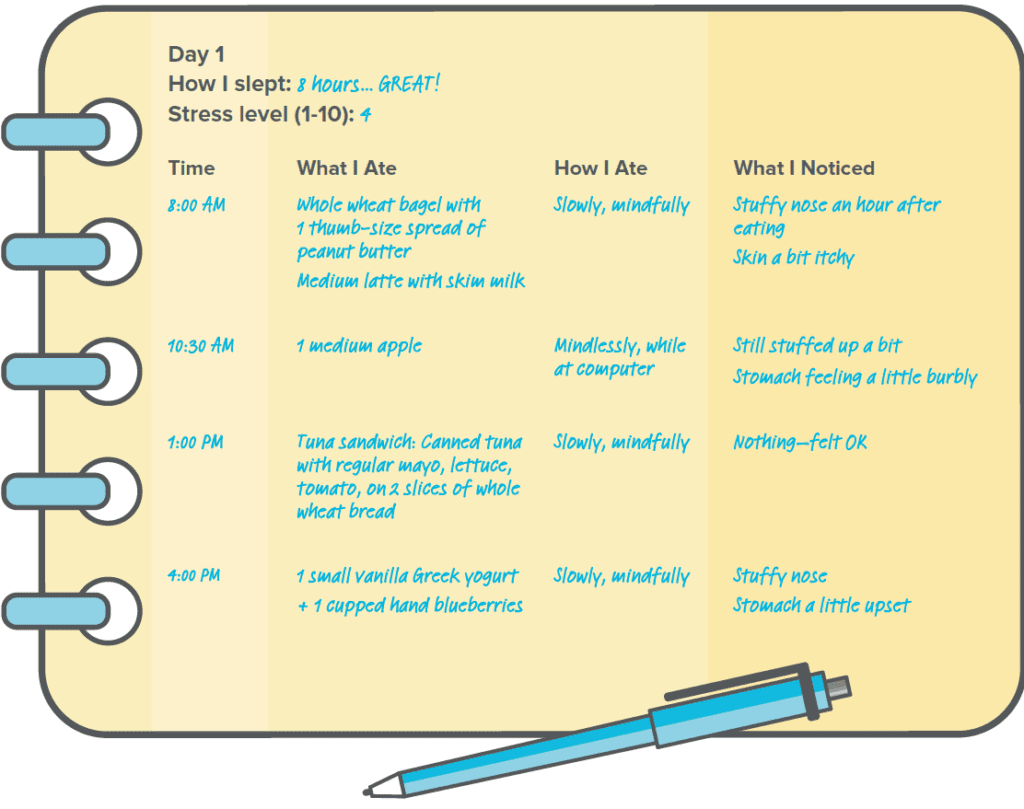
When clients come to me with GI symptoms, I use two different tools to help them connect what they eat with how they feel.
Tool #1: Food journaling
For roughly a month, my clients keep track of:
- What they eat and drink
- How they eat (for example, wolfing down fast food while driving to an appointment vs. slowly savoring a home-cooked meal)
- How much they eat (until just satisfied versus stuffed)
- How they feel, and especially bothersome symptoms such as diarrhea, headaches, bloating, and stomach pain
- How they sleep
- Their stress level
Once they have 30 days of data, we take a look at their journal entries in search of patterns.
To highlight those patterns, I like to bring a client’s attention to days when they experienced vexing symptoms, such as stomach upset. Then I ask:
“What do you notice in your journal in the 2 to 3 days leading up to that flare up? See anything interesting?”
If applicable, I also draw attention to any stretches of time when they had no symptoms at all—and I’ll ask the same question:
“What do you notice in the days leading up to this good stretch? Did you do anything differently during those days that you didn’t do in the days leading up to the flare up?”
This journaling exercise helps people identify sensitivities as well as see they may not have as many sensitivities as they thought.
For example, after looking over their journal, a client might say, “Whoa, I accidentally had dairy on Sunday, and I didn’t have any diarrhea the next day. That’s really weird. But I did have diarrhea just about every day this other week—and I was eating perfectly then. But I was super stressed out. Do you think there’s a connection?”
Want to try this with yourself or a client? Download this free Food and Feelings Journal to get started.
Tool #2: The elimination diet
Elimination diets work a lot like a science experiment to help people identify foods that lead to a wide range of bothersome symptoms. And they do pretty much what the name suggests: exclude certain foods for a short period of time—usually three weeks.
After three weeks, clients then slowly reintroduce specific foods one at a time, each reintroduction spaced a few days apart. As they do so, they monitor their symptoms for possible reactions. Unlike food sensitivity blood tests, elimination diets are the gold standard for identifying food sensitivities.
The problem with elimination diets? They take time and effort.
Do I wish I had a fancy, high tech, super science-y way (like a blood test) to give clients a definitive answer? Absolutely. I do. Because a fancy blood test is easier (for most people) than food logs and elimination diets.
Right now, however, this trial and error approach to testing out different foods is the best we’ve got.
But… we have a tool that makes it easier: Precision Nutrition’s FREE ebook, The Ultimate Guide to Elimination Diets.
This easy-to-use resource includes extensive food lists, recipes, and complete how-to instructions—everything you need to know to try an elimination diet with yourself for a client. (And like I said, it’s 100 percent free.)
How to talk to clients about food sensitivity testing
If you’re a nutrition coach, maybe you’ve had this experience: A client tells you that a food sensitivity test just revealed they can’t eat 47 different foods.
Maybe it’s a young parent who’s already at wit’s end trying to find dinners that all three kids will eat.
“It’s hard enough to cook for my family and make it nutritious and now I have 47 things on my list that I can’t eat anymore,” the client says. “What am I supposed to do?”
Despite my reservations about food sensitivity blood tests, I never start by debunking someone’s test results. That would just make them feel more confused, and possibly alienate them.
Instead, I say something like this:
“If you want to jump in and cut those foods out, we can start there. But, if you don’t mind, I’d love to talk about where you’re eating, why you’re eating, and how you’re eating. Because it’s all connected to what you’re eating and how you feel..”
From there, I usually ask clients a lot of questions:
- How long does it take you to eat your meals?
- What’s your sleep like?
- Do you usually eat at home… or do most meals happen somewhere else, say in the car?
- How would you describe your stress level?
This conversation often opens the door to food journaling. That’s key, because, as I mentioned earlier, a food journal can help clients see—for themselves—what triggers symptoms, and what doesn’t.
For people with multiple food sensitivities, this tool makes meal-planning easy.
Let’s circle back to the parent I mentioned in the previous section. How do you help someone who—legit or not—has a “can’t eat” list that includes 47 foods?
Shine a spotlight on everything they can eat rather than emphasizing what they can’t.
To do so, I print out lists of foods in the following categories: lean proteins, veggies, smart carbs, and healthful fats. Working together with a client, we circle all of the foods they can eat.
Then I ask clients to pick their favorite 10 to 15 in each category.
Once they know their favorites, they can scour cookbooks and cooking sites for recipes and meal ideas that feature those ingredients. (Psst: The local library often stocks all the cookbooks they need.)
Knowledge really can be life-changing.
I’m happy to tell you that my latest scans detected no evidence of cancer in my body. Even better, I now know I can safely eat many, many foods that I once thought were off-limits for me.
Like Brussels sprouts, which happen to be one of my all-time favorite vegetables. Oh, and chocolate. I’m definitely happy that food has come back into my life.
This bears repeating: Most people with digestive problems don’t have cancer. Unlike me, they may have a food sensitivity or two.
Or maybe they don’t have a food sensitivity at all—but rather one of the six (common) issues that mimic food sensitivities.
Our psychological state and our ability to manage our stress has a much bigger impact on digestion than most people realize.
And whether they have a sensitivity or not, many people might be avoiding a lot of foods they could be eating. And they’re living in fear that the meal they just consumed might have them racing to the nearest bathroom.
For these people, food journaling and elimination diets can not only save them money, they can be illuminating, and empowering. These free tools can help them enjoy eating (and life!) all over again.
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We'll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)


Share