In this week’s case study, Doctor Detective meets a man who’s lost his mojo: he’s always tired and has lost his sex drive. We discover that low testosterone is only part of the picture — the other part involves diet and sleep. Before giving out any medication, Doctor Detective tries some simpler — and safer — options first.
++
Eat less and exercise more. It’s generally a great prescription for improving health and improving body composition. However, it doesn’t always work.
Eat less and exercise more. It’s generally a great prescription for improving health and improving body composition. However, it doesn’t always work.
Even with an awesome exercise plan and a rock-solid diet, some people suffer from mysterious symptoms and complaints that seem puzzling, given how much effort they put into their fitness and health.
When we meet clients who have problems that exercise and nutrition — not to mention their own doctors — can’t seem to solve, we know there are only a few experts on the planet to turn to. One of them is Spencer Nadolsky.
Dr. Nadolsky is a doctor of osteopathic medicine who’s also studied exercise physiology and nutrition. An academic All-American wrestler in university, he’s still an avid exerciser and brilliant physician who practices what he preaches to patients -– treating preventable diseases first with lifestyle modifications (instead of prescription drugs).
When clients have nowhere else to turn, Dr. Nadolsky turns from a cheerful, sporty doctor into a meticulous, take-no-prisoners forensic physiologist. He pulls out his microscope, analyzes blood, saliva, urine, lifestyle – whatever he has to, in order to solve the medical mystery.
When Dr. Nadolsky volunteered to work on a regular case study feature with us, we jumped at the chance. By following along with these fascinating cases, you’ll see exactly how a talented practitioner thinks. You’ll also learn how to improve your own health.
In today’s case, we’ll meet a client who came to Dr. Nadolsky with a single complaint: low mojo. Upon further investigation, Dr. Nadolsky discovered low testosterone. Straightforward, right? Just prescribe some testosterone and send him on his way.
But not so fast. Instead of treating with testosterone replacement, Dr. Nadolsky found another problem – the real root of the testosterone problem. And with a few lifestyle modifications, he helped the client get his mojo back.

The client
If you want to get real personal real fast with your doctor, have a conversation about testosterone. As a health care provider, when I’m examining someone with hypogonadism (low testosterone), the discussion becomes intimate very quickly, because I have to distinguish between plain old “loss of mojo” and actual symptoms of low testosterone.
Such was the case with Cameron, a 36 year old male, who came to my office asking for testosterone.
Cameron was morbidly obese — Class 3 to be exact, which is a BMI of over 40. He explained to me that he was “tired all of the time” and that he’d lost most — if not all — of his sex drive. He and his wife agreed that he ought to be on some sort of testosterone prescription.
A quick examination of Cameron suggested that he had good reasons not only to be tired, but hypogonadal. “Hypo” refers to “low”, while “gonadism” refers to the output of the reproductive organs — in the case of men, obviously, the testes.
But it’s important not to misdiagnose. I have to go testosterone hunting in my evidence collection. That means asking about morning erections, sustaining erections, and how full the erections are, along with questions about libido. For both men and women, testosterone is deeply connected to emotional and physical wellbeing. So, we’ve gotta keep the small talk to a minimum and get right to business.
The client’s signs and symptoms
Physical
I examined Cameron when he came into my office. For being over a BMI of 40, his blood pressure was actually normal (120/78). His pertinent positive physical findings were an increased waist circumference (50 inches), increased neck circumference (20 inches), and testicles that were the size of marbles.
Medical history
The history is just as important as the physical. Cameron described the following:
Loss of strength in gymThyroid, anemia, sleep issues, testosterone
| Signs / Symptoms | My thoughts – potential issues |
|---|---|
| Tired all day | Thyroid, anemia, sleep issues |
| Loss of libido | Thyroid, low testosterone, increased estrogen |
| Unable to lose weight | Poor diet, poor exercise, poor sleep, thyroid, high cortisol, testosterone |
Cameron confessed that he ate only one meal per day: a lot of ”fried chicken, some mashed potatoes, and maybe some greens.” I made a note of this, but resolved to keep digging.
If he’s this fatigued, how’s his sleep? He said he got about 6-7 hours of sleep per night. When I asked him if he snored he said, “Nah, I don’t think so.” Quietly, I thought of sleep apnea, especially given that his neck was over 18″ around. I was suspicious, but he said he slept well. I took this at face value for the time being.
The tests and assessments
Symptoms can point us at a hypothesis, but to make a true diagnosis of hypogonadism, one should test morning total testosterone twice — once to screen, and once to confirm.
There’s a lot of overlap in the symptoms for hormonal dysfunctions — thyroid, adrenal, and gonadal issues (among others) can look similar. So it’s important to check them all using blood or salivary tests.
These tests are simply for screening purposes. Some doctors like to shotgun lab testing, but this can be very inefficient and sometimes can take you in the wrong direction. It is very important to hone in on symptoms and start with a few tests. However if you don’t find anything wrong at first, this doesn’t mean the patient is cleared just yet. It means you might not have ordered the right tests.
Test results
Blood chemistry panel
These were Cameron’s pertinent lab findings:
| Marker | Result | Lab Reference Range | Thoughts |
|---|---|---|---|
| Fasting glucose | 84 mg/dL | 65-99 | I figured this would be higher since he has a high risk of insulin resistance. But good nonetheless. |
| Hemoglobin | 15.1 g/dL | 12.5-17.0 | No sign of anemia |
| Hematocrit | 44.5% | 36.0-50.0% | No sign of anemia |
| WBC | 4.6 x10^3/L | 4.0-10.5 | Borderline low – possible immune suppression, but probably not. |
| MCV | 86 fL | 80-98 | No sign of anemia. |
| Total testosterone | 268 ng/dL | 348-1197 | Definitely low. |
| TSH | 1.850 uIU/mL | 0.450-4.500 | This would not throw any red flags up at this point. This is simply a screening tool and if I suspected the thyroid I would get more thyroid labs. |
Cameron’s symptoms were definitely cause for concern, and his intuition of low testosterone was correct. His total testosterone was indeed below the normal range, but why?
At this point, some doctors might’ve thrown some testosterone replacement at him and called it a day. However, Cameron had risk factors that might have caused him to have low testosterone (obesity/lifestyle habits). If we could fix those other risk factors, maybe his testosterone would come back up. On the other hand, it might just be that his testicles just didn’t produce testosterone very well.
Either way I wanted to have him back for more testing as well as questioning.
Cameron’s second visit
The second time Cameron came into my office, he brought his wife with him. I explained to both of them the results of the tests, and that he truly does have low testosterone. I also explained that I didn’t want to just start him on testosterone replacement because then he would have to be on it the rest of his life, and that we might be able to fix it without drugs.
He and his wife were intrigued by the notion of increasing testosterone naturally. I explained the relationship behind healthy dietary habits and testosterone. His wife, the household cook, insisted that her food was healthy. Discussion closed.
I tried the sleep angle. Cameron claimed that he slept well and didn’t snore. This time however, his story didn’t check out. “Cameron sounds like a motocross bike when he sleeps!” exclaimed his wife. Cameron looked shocked. He’d had no idea.
I explained to both of them that instead of getting another testosterone level, I wanted to get a sleep study. They obliged and left with a prescription for the study.
Sleep study results
Here’s a snippet of the report from the sleep study.
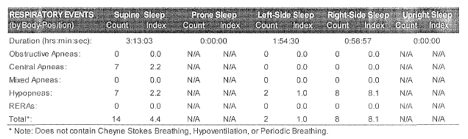
The study notes from the pulmonologist say: “Mild to moderate sleep apnea composed predominantly of hypopneas and without prolonged or severe desaturations.” Hypopnea is shallow or slower breathing, compared with apnea which is no breathing; desaturation refers to a low oxygen level. Translation: some reduced breathing, but it wasn’t serious… yet.
I explained to Cameron that they wanted to do another sleep study with a CPAP machine (a machine that will keep the airways open during the night so you can get the oxygen you need — CPAP stands for “continuous positive airway pressure”). Cameron refused to do this. Either way, he said, “I’m not using a CPAP at home.”
We were at a bit of an impasse, until I really looked at the report. It looked as though Cameron only had 2 hypopneas while lying on his left side. I told him to only sleep on his left side for this week, then call and tell me how it went.
Amazingly enough, Cameron called back later in the week telling me he not only feels a little bit better, but also that his wife said that he snored much less!
I have read studies about sleep position alleviating sleep apnea, but I wasn’t sure if it would be enough to help Cameron. Plus, if he could lose weight, the sleep apnea would likely resolve.
Unfortunately, although weight loss is a simple yet crucial treatment for sleep apnea, folks who have sleep apnea are in a bit of a catch-22. They struggle with a few extra problems:
- they’re usually too tired to work out, which leads to lower activity;
- they have increased cravings for refined carbohydrate-rich foods, which leads to over-eating; and
- they also have sky high nightly cortisol, which can make it hard to fall asleep,
All of this, of course, makes it even harder to lose weight.
Sleep apnea and hypogonadism
To add insult to injury, sleep apnea is one cause of secondary hypogonadism through the mechanisms related to the above (e.g. high cortisol).
And more insult to more injury, low testosterone can also come from carrying excess body fat, especially visceral fat. With increased adipose tissue (aka fat) comes higher aromatase, which converts testosterone to estrogen. This means his pituitary secretes less luteinizing hormone (luteinizing hormone, or LH, is what stimulates the testes to make testosterone).
So: testosterone is low; the testosterone that is there is being converted to estrogen, and the pituitary doesn’t know it needs to kick-start the production system.
There are a few other mechanisms that are out of the scope of this article, but in essence: excess weight can cause both low testosterone and sleep apnea.
So what did I do?
The prescription
Some doctors have their patients on what we call “polypharmacy,” which basically means a lot of meds. This can be problematic for obvious reasons (interactions, weight loss inhibition, etc.), but it also dramatically drops compliance (think Lean Eating — one habit at a time.). For me, less is more.
Fix #1 – Sleep position
Cameron could lessen his sleep apnea just by changing how he lay in bed. Since he refused a CPAP machine, this was the best shot we had at alleviating this issue. I told him to sleep on his left side, and instructed his wife to wake him up and make him turn over if he switched sides during the night. I figured this probably wouldn’t be as necessary if he was able to lose some weight — the issue might resolve itself.
Fix #2 – Meal frequency and quality
There was much improvement to be had here, but small and simple changes are the way to go. I told him he could still have his fried chicken, but instead of bread crumbs he must use almond flour/meal. I told his wife that he must also have double the green vegetables at night and half of the starches that he is used to. They were very confident (rating their confidence as a 9 on a scale from 1 to 10) that this could be done.
I wanted to add another meal to Cameron’s day so he wouldn’t feel the need to binge at night. The easiest choice was adding in a Leaner Living MRP for breakfast, which would give him the quality protein, fibre, and vitamins/minerals he was missing without many added calories.
These are the only things we changed at first. I didn’t want to bombard Cameron in the beginning, because it rarely ever works. He was to report back via email once a week for close follow up. I didn’t want to change exercise habits right now because of how tired he was. I figured that if this plan worked, we could start adding in the exercise.
The outcome
After one month of following this plan, Cameron brought his logbook back with his X’s and O’s on each day he did or did not complete the new habits I gave him. I was excited to see he was able to keep an 86% adherence rate.
Just looking at Cameron I knew things had changed. His eyes were not nearly as bloodshot as they were before, and his clothes were definitely fitting better.
Cameron had lost a half inch in his neck circumference as well as a solid 9 pounds. While weight and circumferences matter, I wanted to know more about his sex life and life in general. Both Cameron and his wife smirked. “My libido is up a little bit,” he announced. He was also feeling better and more productive at work.
This was great news. I decided to verify his self-assessment with another morning total testosterone and he was to follow up in another month, going with the same sleep and diet plan, plus a small workout program I gave him.
The total testosterone came back at 390 ng/dL, which was still somewhat low, but now within the normal limits! Correlating this with his clinical improvement, it was clear we were on the right track.
Ensuring ongoing progress
After further followups, Cameron had lost a total of 40 pounds and had a moderate boost in his testosterone (upwards of high 400s and low 500s). I will continue to help him lose weight and modify his plan accordingly.
Now what if I had just haphazardly started him on testosterone replacement without finding the underlying issue?
For one, he would have probably been on it for the rest of his life unless we treated the underlying problem along with a small amount of replacement. If that doesn’t sound bad enough, testosterone replacement can actually make your sleep apnea worse! So maybe I would have made him feel slightly better in the beginning, but I would have seriously deteriorated his health in the long run. Powerful stuff!
Summary
Cameron came to us with what he thought was low testosterone along with fatigue. He was right, but we first ruled out other entities that cause these same symptoms. We also found the cause of his low testosterone and were able to treat it with small changes (sleep position and diet). He responded very well and has had remarkable results.
So what can we take away from Cameron’s story?
- When someone complains of fatigue and loss of libido, there can be multiple reasons for this. Many symptoms overlap and it is important to distinguish these.
- Just because you have low testosterone doesn’t mean you need to take testosterone replacement. There can be many underlying problems that — once corrected — can result in a normal testosterone.
- Sleep apnea is very prevalent. If someone snores, they need to be checked for sleep apnea. Some folks might not be as lucky as Cameron; in their case, changing sleep position alone may not be enough. They might need a CPAP machine in order to alleviate the apnea/hypopneas.
- Losing fat can help a whole host of medical problems and is not just for looking good. But sometimes you need to correct underlying issues before the patient/client can lose weight.
Eat, move, and live… better.©
Yep, we know… the health and fitness world can sometimes be a confusing place. But it doesn’t have to be.
Let us help you make sense of it all with this free special report.
In it you’ll learn the best eating, exercise, and lifestyle strategies — unique and personal — for you.

Share