In this week’s case study, Dr. Detective meets a middle-aged man with mysterious abdominal pain and shows us that the liver can be just as vulnerable to unhealthy foods as it is to too much alcohol.
Eat less and exercise more. It’s generally a great prescription for improving health and improving body composition. However, it doesn’t always work.
Even with an awesome exercise plan and a rock-solid diet, some people suffer from mysterious symptoms and complaints that seem puzzling, given how much effort they put into their fitness and health.
When we meet clients who have problems that exercise and nutrition — not to mention their own doctors — can’t seem to solve, we know there are only a few experts on the planet to turn to. One of them is Spencer Nadolsky.
Dr. Nadolsky is a doctor of osteopathic medicine who’s also studied exercise physiology and nutrition. An academic All-American wrestler in university, he’s still an avid exerciser and brilliant physician who practices what he preaches to patients -– treating preventable diseases first with lifestyle modifications (instead of prescription drugs).
When clients have nowhere else to turn, Dr. Nadolsky turns from a cheerful, sporty doctor into a meticulous, take-no-prisoners forensic physiologist. He pulls out his microscope, analyzes blood, saliva, urine, lifestyle – whatever he has to, in order to solve the medical mystery.
When Dr. Nadolsky volunteered to work on a regular case study feature with us, we jumped at the chance. By following along with these fascinating cases, you’ll see exactly how a talented practitioner thinks. You’ll also learn how to improve your own health.
In today’s case, we’ll meet a middle-aged man whose mysterious abdominal pain is ultimately traced to his liver.

The client
Walter, a 49-year-old male, came to my office for “abdominal pain.”
I’d inherited Walter from another doctor who had left the practice. This was our first meeting, but I knew he was being followed in our clinic for his high blood pressure.
The client’s signs and symptoms
Looking at Walter’s records, I could see he’d never been diagnosed with anything besides slightly elevated blood pressure and high triglycerides. Apart from that, he’d visited the office with a few colds and some back strain. According to the records, he’d never complained of any abdominal pain.
Figuring out the cause of his problem was going to take some sleuthing.
As always, I checked his vital signs. His blood pressure was still mildly elevated at 132/87, his weight was 223 (BMI 32), and his waist circumference was 43 inches.
As I walked into the room to meet him, I was running through the possibilities:
| Signs / Symptoms | My thoughts – potential issues |
|---|---|
| Elevated blood pressure | Weight issues, stress, sleep problems, atherosclerosis, kidney issues, thyroid, adrenal. |
| Elevated body weight/waist circumference | Likely lifestyle factors, could be thyroid related (but not likely), metabolic syndrome/insulin resistance. |
At first glance, none of the things I noticed seemed linked to abdominal pain.
The only medication Walter was taking was lisinopril (an angiotensin converting enzyme inhibitor) for his high blood pressure. He wasn’t taking any supplements.
Walter told me his belly pain was dull, mostly on the right side, and had been occurring for a few months. On a scale of 1-10 with 10 being the worst pain he had ever experienced, this pain was a 3.
The pain didn’t radiate anywhere and it wasn’t located in a specific spot. He also said the pain didn’t change with food or bowel movements. Nothing really made it better or worse.
Hmmm. This wasn’t much for me to go on.
Making a differential diagnosis wasn’t going to be easy. His history wasn’t pointing to a definite answer.
While chatting with him some more, I started pushing on his belly. I couldn’t elicit any pain when pressing, and his bowel sounds were normal. I didn’t think his liver was enlarged. There was no sign of gallbladder disease. He didn’t have a family history of any pancreatic or hepatic problems.
Walter mentioned that he drank alcohol, but quite irregularly – at maybe 3 times a year. He ate the average American high carb / high fat diet and exercised as much as the average American – which of course isn’t much. It was possible that lifestyle factors were playing a role in his pain, but I wasn’t so sure yet.
It was time to get some labs.
The tests and assessments
Even though there were no obvious signs of liver, pancreas, or gallbladder problems, I needed to investigate further, so I ordered CBC (Complete Blood Count), CMP (comprehensive metabolic panel), lipase, and GGT (Gamma-glutamyl Transpeptidase) test panels.
The test results
Blood chemistry panel
These are Walters’s pertinent lab findings:
| Marker | Result | Lab Reference Range | Thoughts |
|---|---|---|---|
| Fasting glucose | 115 mg/dL | 65-99 | Impaired fasting glucose. Insulin resistance is present. |
| AST | 47 IU/L | <35 | Some sort of liver inflammation/damage. |
| ALT | 52 IU/L | 10-35 | Some sort of liver inflammation/damage. |
| Albumin | 3.6 | 3.5-5 g/dl | On the lower end. Might not be eating enough protein or his liver isn’t working well. |
| Alkaline phosphatase | 140 IU/L | 44-147 | On the higher end. Could be related to the liver inflammation. |
| GGT | 70 IU/L | 15-80 | On the higher end. Could be related to the liver inflammation. |
| Platelets | 160 x10^9/L | 150-400 | On the lower end. Could be due to the liver not working well. |
| Direct bilirubin | 0.2 mg/dL | <0.4 | Normal. |
| Total bilirubin | 0.6 mg/dL | 0.3-1 | Normal. |
| Prothrombin time | 13 seconds | 11.4-14.2 | Normal. This is a measure of how well your blood clots, but since prothombin is made in the liver, it can show liver function. |
| Lipase | <160 | 30-210 U/L | Normal. This is a measure of how well your blood clots, but since prothombin is made in the liver, it can show liver function. |
Walter’s labs suggested that he had some liver inflammation. When I see this, I’ll routinely run a hepatitis panel that searches for Hepatitis B and C.
Walter’s hepatitis tests came back negative. This was great news – but we still didn’t know what was going on.
When the liver enzymes look like his, alcohol abuse should always be suspected (although the AST:ALT ratio would likely be greater than 1 in alcohol related hepatitis). But Walter was adamant that he rarely drank.
Medications and supplements can also cause liver damage, but again, Walter wasn’t taking anything other than lisinopril for his blood pressure.
I rolled up my sleeves for some more investigations.
My next thought was that Walter might have hemochromatosis (iron overload disease). I ordered iron studies, but his ferritin (shows iron stores) and Transferrin/TIBC/iron levels were all normal. Finally, I ordered a right upper quadrant ultrasound – which, you guessed it! – also came back normal.
The one possibility that kept returning to me was the idea that Walter was suffering from non-alcoholic fatty liver disease (NAFLD for short). But the only way to confirm this absolutely would be a liver biopsy — obviously not something to be taken lightly. There are also special ultrasounds and MRIs available, but these may or may not show anything.
We were at an impasse. But, given Walter’s metabolic syndrome, NAFLD seemed a plausible diagnosis. I decided to run with it. It was time for some lifestyle changes and powerful supplements.
A quick overview of NAFLD
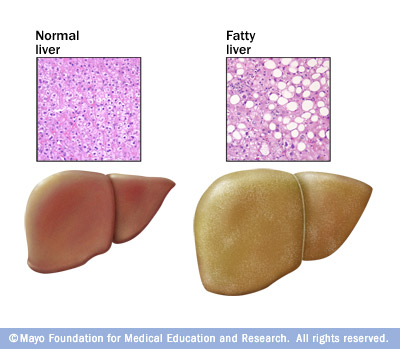
We commonly associate liver disease with drinking too much. And indeed, drinking too much certainly isn’t good for liver health. Chronic over-consumption of alcohol can lead to inflammation and fibrosis (cellular hardening) as well as fat deposits (steatosis).
But many people don’t know that the same problem can happen with obesity and the metabolic syndrome (which includes insulin resistance and poor processing of blood lipids along with system-wide inflammation). When we have an abundance of body fat, it doesn’t just accumulate on our butts and bellies — it builds up around and inside our internal organs as well. Because the liver is such a major cellular signaling, switching, and processing centre, it’s often one of the hardest-hit organs when people consume a poor diet and carry too much body fat.
Although heart disease and stroke get much of the media attention, experts suspect that hepatic steatosis — aka non-alcoholic fatty liver disease — is one of the least commonly known yet most frequent effects of obesity and poor nutrition.
Walter’s second visit
On Walter’s follow-up visit, I explained the situation to him. We couldn’t know for certain without that liver biopsy, but his insulin resistance was probably contributing to liver disease. Instead of doing its job of breaking down fats, his liver was actually holding onto them, regularly bathing in a cocktail of free fatty acids. Not good.
Walter understood and was eager to fix the problem. I told him it wasn’t going to be easy, but if he stuck with Dr. Detective for the next few months, together we could take care of it, We’d start with a gradual weight loss plan and some supplements.
Since Walter’s diet was far from optimal, we had plenty of options for improvement. The only question would be where to start.
The prescription
Fix #1 – Change the diet
Walter loved soda and sweet tea. But giving those up would be a relatively easy change, so we decided they had to go. We also agreed he needed a little more protein in his life.
Yes, I was taking a risk asking Walter to adopt two new habits at once. But he was motivated. And I figured if he could focus on drinking calorie-free beverages and adding lean protein for the next couple of months, we’d be off to a great start.
Walter loved coffee. Since coffee has been shown to be beneficial in NAFLD, I told him to feel free to enjoy it – as long as he sweetened it with stevia.
Fix #2 – Fish oil
Walter had a history of hypertriglyceridemia (high triglycerides) so I told him to use a hefty dose of fish oil to help with this. Fish oil hasn’t been shown to help with NAFLD (yet) but it couldn’t hurt. Along with reducing his carbohydrates (by cutting out the sugar-laden sodas), this would be key to changing his overall metabolic profile.
Fix #3 – Berberine
Because berberine can help with insulin resistance, and some small trials have suggested it might be beneficial for NAFLD, I added it to Walter’s regime.
The outcome
For the next few months, Walter and I communicated through email. He had his good days and bad days, but overall he made some significant lifestyle improvements.
At the end of 3 months, Walter returned to the office. His abdominal pain had mostly disappeared. Bingo!
But he was even more excited to report that he had lost 7 inches around his waist. He’d also lost a total of 18 pounds since I’d first seen him. That may not sound like much, but to Walter it represented an enormous difference.
To see if the inner changes matched up with the visible change, we repeated his liver enzyme labs. Both came back at around 30 IU/L — within normal limits.
Today, Walter continues to see me in the clinic for weight loss . He has also started going to the gym, where he works out 3-4 times per week. Having started by changing just two habits, Walter is well on the way to a healthier future.
Take-away
So what can we take away from Walter’s story?
- Abusing alcohol is not the only way to ruin your liver. Without intervention, Walter’s liver could have ended up just as diseased as an alcoholic’s.
- If you’re suffering from vague abdominal pain (or any abdominal pain) and it lasts for more than a week or two, you should visit your doctor. Don’t neglect the health of your vital organs!
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.

Share