Blood tests (aka blood work) can show us, obviously, what’s in our blood. (And, by extension, what’s in our bodies). That’s because blood gives us insight into what we can’t see from the outside.
In this article we outline how it works and what you need to know.
What is blood work?
Blood is a transport system for the body. We carry all kinds of things in the approximately 5 litres of blood that circulates constantly through our system.
Blood tests, aka blood work, can show us what’s in our blood — and by extension, what’s in our bodies. Blood can also show us changes in our bodies that we might not be able to see from the outside — such as our blood sugar levels or nutritional status.
Thus, we can use blood work to assess overall health, and it can give us a much more accurate and objective snapshot of wellness than “Gee, I think I had some veggies yesterday” or “I feel fat today”.
How is blood work done?
We get blood for testing from:
- Capillary skin puncture (finger stick)
- Dried blood samples
- Blood drawn from an artery
- Blood drawn from a vein (most common)
- Bone marrow aspiration
What happens to blood after it’s drawn?
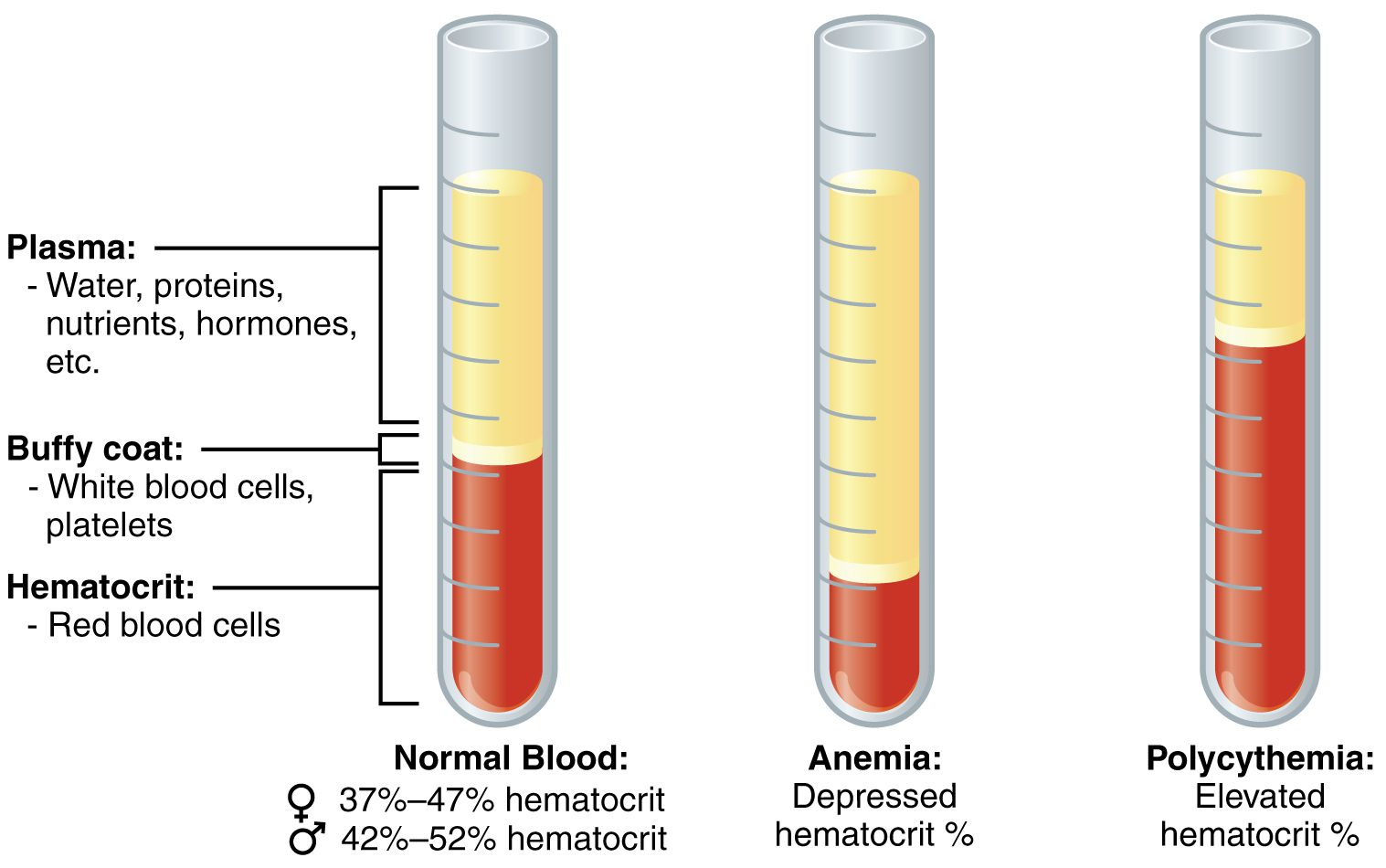
Blood is analyzed in a lab. The blood is put into a centrifuge and spun until it separates.
Reference ranges
Then, technicians compare results to a “reference range.” The reference range is the range of expected values for each test listed.
Expected ranges used in lab analyses include 95% of the “healthy” population. So, 95% of healthy people would have lab values within these ranges. This range varies depending on the lab, region (e.g. US vs EU) and type of blood component.
A number above or below this reference range can give valuable diagnostic information about body systems. High and low values are especially useful when taken in context with other symptoms, lifestyle factors, and tests.
Variation in results and ranges
Lab values vary for each person and must be assessed relative to other factors. While reference ranges are established after testing a large number of healthy people, everyone is slightly different.
Blood analyses vary based on:
- Time of year
- Posture/positioning
- Food/fluid intake
- Stress
- Medication/supplement use
- Alcohol
- Smoking
- Exercise/physical activity
- General tests
Blood work: the tests
The basic test
A general lab ordered by a physician is typically called SMAC-20, SMA-20, or Chem-20.
This basic test looks at 20 different parts of the blood including levels of certain minerals, proteins, etc. This test is standard and should be done, although it’s not very telling of one’s overall health profile.
Beyond the basic SMAC-20, there are many different blood tests you can request. Highlighted below are some of the most useful tests.
Cardiovascular tests
| Test | What it is | Higher with | Lower with |
| Total cholesterol | Cholesterol is necessary for building brain and nerve cells, along with various hormones.Too much of it floating around the blood is associated with cardiovascular disease (CVD). Some experts claim that if you keep this under 150 mg/dL – you’ll be “heart attack resistant.” | Cholestasis, nephritic syndrome, chronic renal failure, hypothyroidism, alcoholism, a diet high in cholesterol and fat, obesity, pregnancy. | Myeloproliferative disease (e.g., polycythemia vera, thrombocytosis, myelofibrosis, chronic myelogenous leukemia), hyperthyroidism, malnutrition, some lung diseases, warmer months, sitting (versus standing), certain drugs, estrogen medications. |
| Low density lipoprotein (LDL) | This compound carries cholesterol to body cells from the liver. Small, dense LDL levels have a strong association to CVD. | Overeating (and most folks overeat processed fats, sugars, and refined grains), hypothyroidism, nephrotic syndrome, multiple myeloma, hepatic obstruction, anorexia nervosa, diabetes, renal failure, porphyria, pregnancy, androgen use. | Tangier disease, hyperthyroidism, anemia, Reye’s syndrome, inflammatory joint disease, estrogen use. |
| Apoplipoprotein A & B | These are surface proteins of lipoprotein particles. Apo A is the main component of HDL. Apo B is the main component of LDL. | Apo A: Not significant.Apo B: Diabetes, hypothyroidism, renal failure, hepatic disease, Cushing’s syndrome. | Apo A: Diabetes, renal failure, diets very high in polyunsaturated fat, smoking, some drugs, genetic diseases.Apo B: Malnutrition, plant-based diets, high polyunsaturated fat diets, some drugs, genetic diseases. |
| Lipoprotein (a) (Lp(a)) | This is another sub-fraction of cholesterol. High levels of this are associated with premature heart disease. | Post-menopausal women, African-American race, renal failure/disease, estrogen depletion, hypothyroidism, diabetes. | Not significant – levels might be slightly lower with niacin use. |
| High density lipoprotein (HDL) | This compound carries cholesterol from cells back to the liver. There is a strong relationship between HDL and CVD. The ratio of total cholesterol to HDL is considered a better predictor of heart disease than total cholesterol or LDL. The goal is to have a ratio of 5:1 or lower in men; 4.4:1 in women. An optimum ratio is 3.5:1 or lower in men, 3.4:1 or lower in women. | Lots of exercise for many years, estrogen use, low levels of alcohol consumption. | Diabetes, cholestasis, renal failure, obesity, sedentary behavior, certain drugs, insulin resistance. |
| Triglycerides | Fat in the blood levels predict the body’s ability to metabolize fat. When triglycerides are under 100, the LDL calculation is usually inflated. The triglyceride to HDL ratio might be the single best predictor of heart disease risk. A ratio above 4:1 is cause for concern. The goal is a ratio of 2:1; the lower the better. | CVD, liver disease, alcoholism, renal disease, hypothyroidism, pregnancy, birth control medications, smoking, obesity, diabetes, gout, anorexia nervosa, a recent meal with fat. | Malnutrition, hyperthyroidism, some lung diseases, strenuous exercise, a lean body. |
| C-reactive protein (CRP) | A marker for low grade inflammation. Useful in predicting CVD. | Pain, fever, infection, inflammatory bowel disease, arthritis, autoimmune disease. | Not significant – can be an indication that inflammation is decreasing. |
| Homocysteine | An amino acid found in small amounts in the blood resulting from the synthesis of cysteine from methionine. Only cleared from the body with adequate blood levels of vitamin B12, B6 and folate. Elevations of homocysteine are associated with CVD. | Folic acid deficiency, vitamin B12 deficiency, vitamin B6 deficiency, heredity, older age, kidney disease, male gender, certain medications. | Not significant. |
Liver function tests
| Test | What it is | Higher with | Lower with |
| Alkaline phosphatase |
If the bile duct is blocked (cholestasis), this enzyme gets backed up and spills into the bloodstream. Values can help to evaluate bone health since elevated levels show active bone growth or inflammation due to damaged or healing bones. If elevated in conjunction with GGT, we have a liver issue. | Younger age, fatty liver, pregnancy, obstructive jaundice, liver disease, diabetes, alcohol consumption, eating a fatty meal, gallbladder conditions, bone growth, damaged bones, Paget’s disease, vitamin D deficiency. | Not significant. May indicate celiac disease, malnutrition, scurvy, or magnesium/zinc deficiency. |
| GGT | A cholestatic liver enzyme. If the bile duct is blocked (cholestasis), this enzyme gets backed up and spills into the blood stream. Evaluates liver and gallbladder function, but is also found in kidneys. Helpful when alkaline phosphatase levels are elevated. | High alcohol intake, various liver disorders, stress, excess body fat, exercise, some drugs.If GGT and alkaline phosphatase are elevated, it’s likely a liver disorder. | If GGT is low and alkaline phophatase is elevated, it’s likely a bone disorder (instead of a liver disorder). Otherwise, low GGT isn’t significant. |
| AST/SGOT | An enzyme found mainly in the liver, heart, and muscles – organs with high metabolic activity. | Liver damage, heart damage, muscle damage, high body fat, diabetes, mononucleosis, pregnancy, hypothyroidism, shock, some drugs. | Azotemia, dialysis, vitamin B6 deficiency. |
| ALT/SGPT | Enzyme found mainly in the liver. | Damage to the liver from alcohol, inflammation, increased body fat, mononucleosis, some drugs, heart attack, aspirin, strenuous exercise. | Not significant. |
| Bilirubin | This is a normal, yellow fluid metabolic by-product of red blood cell breakdown that must be cleared by the liver. | Bile flow impairment, carcinoma, liver disease, high levels of red blood cell breakdown, prolonged fasting, anorexia nervosa, niacin supplementation, some forms of anemia.Note: Exposing a blood sample to 1 hour of sunlight can decrease bilirubin. | Rare and not significant.Note: Foods with lots of orange color (carrots, yams) can increase the yellow hue in serum and falsely increase bilirubin levels if tested with a spectrophotometer. |
| Ammonia | The end product of protein metabolism. The liver normally removes ammonia via portal vein circulation with conversion to urea. Levels in our blood dramatically influence acid/base balance and brain function. | Reye’s syndrome, liver disease, gut hemorrhage, renal disease, inborn errors of metabolism, excessive protein intake, some drugs, intense exercise, smoking, alcohol, constipation, gut infection. | Not significant. |
Kidney function tests
| Test | What it is | Higher with | Lower with |
| Creatinine | This is a metabolic by-product of muscle metabolism that must be filtered by the kidneys. Since muscle creatine breaks down into creatinine, someone with more muscle will have abundant creatine and potentially higher creatinine levels. When there is disordered kidney function, the ability to excrete creatinine diminishes. | Impaired kidney function (along with high BUN), obstruction of the urinary tract, muscle disease, shock, heart failure, dehydration, rhabdomyolysis, high meat diet, hyperthyroidism. | Decreased muscle mass, inadequate protein intake, pregnancy. Low levels usually aren’t cause for concern. |
| BUN (blood urea nitrogen) | Urea is a waste product of protein metabolism eliminated from the body through urine, feces, and perspiration. BUN is a measure for kidney function because if filtration in the kidneys can’t keep up with elimination, kidney function is likely diminished. | Various kidney diseases, heart failure, urinary tract obstruction, gut hemorrhage, diabetes with ketoacidosis, steroid use, circulatory disorders, high animal protein intake, intense exercise, salt or water depletion from sweating, diarrhea, vomiting. | Pregnancy, liver failure, acromegaly, Celiac disease, syndrome of inappropriate antidiuretic hormone (SIADH), malnutrition. |
| Creatinine/BUN ratio | This provides more information about potential kidney problems. | Increased ratio with normal creatinine occurs in: Salt depletion, dehydration, heart failure, catabolic states, gut hemorrhage, high animal protein intake.Increased ratio with elevated creatinine occurs in: Obstruction of the urinary tract, ketoacidosis, prerenal azotemia. | Decreased ratio with decreased BUN occurs in: Tubular necrosis, malnutrition, dialysis, SIADH, pregnancy.Decreased ratio with elevated creatinine occurs in: Some drug use, rhabdomyolysis, muscular folks who are developing kidney failure. |
Thyroid tests
| Test | What it is | Higher with | Lower with |
| TSH | The thyroid has large hormone storage potential and a slow rate of turnover. TSH is secreted by the pituitary gland and stimulates thyroid gland function, leading to the release of T3 and T4. TSH secretion is regulated by T3 and T4 (feedback inhibition) and is stimulated by thyrotropin-releasing hormone (released from the hypothalamus). This test is the most sensitive for primary hypothyroidism. | An under-active thyroid, advanced age, amphetamine abuse. | An overactive thyroid, corticosteroid use, too much thyroid replacement medication. TSH tends to go down later in the day. |
| Free T3 (triiodothyronine) | The fraction of T3 that exists unbound in the blood. | Hyperthyroidism, high altitude, T3 toxicosis. | Hypothyroidism, late stage pregnancy. |
| Total T3 (triiodothyronine) | T3 has three iodine atoms attached and more metabolic action than T4, but the effect is short lived. This test is helpful for diagnosing T3 toxicosis and hyperthyroidism. Not useful for diagnosing hypothyroidism. | Hyperthyroidism, T3 toxicosis, thyroid medication use, heroin use, estrogen use, pregnancy, iodine deficiency goiter. | Hypothyroidism, anabolic steroid use, aspirin, niacin use, fasting, malnutrition. |
| Free T4 (thyroxine) | This only makes up a small fraction of total T4. Free T4 is unbound and available to tissues. It’s metabolically active. | Hyperthyroidism, heparin use, hypothyroidism treated with T4. | Hypothyroidism, chronic illness, pregnancy. |
| Total T4 (thyroxine) | T4 has four atoms of iodine attached. This test shows the total amount of T4, consisting of T4 bound to carrier proteins and unbound T4 available to cells. Bound T4 is inactive. | Hyperthyroidism, high estrogen levels from pregnancy, birth control use, estrogen replacement, hepatitis, lymphoma, heroin use, excessive iodine intake. | Steroid use, liver disease, hypothyroidism, aspirin, nephritic syndrome. |
| rT3 (reverse T3) | If the body is under stress it may convert T4 into rT3 (reverse T3), an inactive form of T3. rT3 can also bind to T3 receptors, blocking actual T3. This allows the body to “turn down” energy levels. T3 and rT3 have an inverse relationship, when there is more of one, there is less of the other. rT3 test results can be indicative of Wilson’s Syndrome. |
Reproductive function tests
| Test | What it is | Higher with | Lower with |
| Testosterone | Responsible for the development of male secondary sex characteristics and sex drive (in both men and women). Secreted by testes, ovaries and adrenal glands. Exists in serum as both unbound (free) and bound. Unbound is active testosterone. Levels are subject to diurnal variation with a peak in the early morning. | For men: Anabolic steroid use, cancer of the testes.For women: Hyperthyroidism, adrenal tumors, androgen resistance, ovarian tumors, hirsutism, polycystic ovaries, some drugs, virilization, hilar cell tumors. | For men: Hypogonadism, Klinefelter’s syndrome, hypopituitarism, liver disease, some drugs, down syndrome, advanced age, alcohol abuse, some drugs.For women: Menopause, ovarian failure. |
| IGF-1 | A growth factor produced by the liver and muscles directly in response to growth hormone. IGF-1 can help evaluate pituitary function and diagnose situations related to growth hormone production. | Increased growth hormone production, puberty, pregnancy, pituitary tumors, obesity. | Deficiency or insensitivity to growth hormone, decreased pituitary function, advancing age, anorexia nervosa, malnutrition, diabetes, kidney disease, liver disease, high dose estrogen. |
| Growth hormone (GH) | A hormone secreted by the pituitary gland in response to exercise, deep sleep, hypoglycemia, glucagon, insulin and vasopressin. GH is essential to the growth process and metabolism. | Gigantism, acromegaly, uncontrolled diabetes, diabetes, fasting, anorexia nervosa, exercise. | Dwarfism, hypopituitarism, obesity, malnutrition, certain drugs/supplements, stress. |
| DHEA/DHEAs | An androgen that can be metabolized into testosterone or estrogen. Released mainly by the adrenal glands – it can also be released by the testes and ovaries. Controlled by ACTH from the pituitary gland. | Adrenal tumors, PCOS, puberty. | Adrenal dysfunction, pituitary dysfunction. |
| Estradiol | An important estrogen involved with sexual development. Produced mainly in the ovaries, but also in the adrenal glands and testes. Levels vary in menstruating women. Useful for diagnosing the reason behind amenorrhea. | Puberty, gynecomastia, ovarian tumor. | Turner syndrome, ovarian failure, rapid weight loss, low body fat, anorexia nervosa, malnutrition. |
| PSA (for men) | A screening recommended for males 40 years or older. PSA is produced by the prostate gland. Normal PSA levels don’t rule out prostate cancer. Nearly 25% of prostate cancers are missed by this lab alone. | Prostate cancer, prostate enlargement. | Not significant. |
Carbohydrate tolerance tests
| Test | What it is | Higher with | Lower with |
| Fasted insulin |
Insulin is a hormone secreted by the pancreas in response to increases in blood sugar, usually following a meal. | Pancreatic tumors, type 2 diabetes, acromegaly, Cushing’s syndrome, obesity (most common cause), diabetes medications, birth control medications. | Type 1 diabetes, hypopituitarism, diabetes medications. |
| Fasted glucose | Blood sugar. High values will occur if someone isn’t fasted. Beyond that, a true high fasted blood sugar indicates insulin resistance. If you are fasted, and your blood glucose is above 126 mg/dL, you have diabetes. | Diabetes, Cushing’s disease, stress, acromegaly, pituitary adenoma, hemochromatosis, pancreatitis, glucagonoma, liver disease, renal disease, vitamin B deficiency, pregnancy, catabolic steroid use, pregnancy, diuretics, obesity, sedentary habits, alcohol use, aspirin use, smoking. | Insulinomas, Addison’s disease, ACTH deficiency, starvation, liver disease, enzyme deficiency disease, reactive hypoglycemia, exercise, anabolic steroid use, acetaminophen use, high hematocrit. |
Protein status tests
| Test | What it is | Higher with | Lower with |
| Albumin and globulin | These are proteins made in the liver and released into the blood. They are useful for evaluating overall health and nutrition status. Globulin fights disease. Albumin makes up about 2/3 of the total protein in the body and keeps water inside blood vessels. | Albumin: Dehydration.Globulin: Severe liver disease, infectious disease, blood disease, autoimmune disease, tuberculosis, multiple myelomas. | Albumin: Malnutrition, overhydration, liver disease, kidney disease, bone fractures, severe injury, inflammation, infection, Crohn’s disease, heart failure, thyroid dysfunction, slow bleeding, pregnancy, bed rest, certain medications.Globulin: Malnutrition, overhydration. |
Vitamin, mineral, acid/base status tests
| Test | What it is | Higher with | Lower with |
| 25-hydroxyvitamin D [25(OH)D] | The amount of vitamin D that has been produced in the body from sun, food and supplements. The half-life is 15 days. This lab can help indicate bone defects. Low levels are associated with immune disorders, CVD and some cancers. | Excessive supplementation or consumption from food. | Dietary insufficiency. |
| 1,25 (OH)2D | This lab is not a good indicator of vitamin D status, as it has a short half life of only 15 hours and levels in the blood are regulated tightly by hormones and minerals. 1,25 (OH)2D only starts to decline when a severe deficiency of vitamin D is present. | ||
| Vitamin B-12 | Also known as anti-pernicious anemia factor. Necessary for red blood cell production, tissue repair, DNA synthesis, nervous system development. | Leukemia, renal failure, liver disease, polycythemia vera, heart failure, diabetes, obesity, COPD, high supplemental intake. | Pernicious anemia, inflammatory bowel disease, tapeworm, hypothyroidism, Zollinger-Ellison syndrome, bacterial overgrowth, dietary insufficiency, malabsorption, increased losses, aging, smoking, alcohol use, pregnancy, birth control medications, high supplemental doses of vitamins A and C. |
| Folic acid | Needed for normal cell function. It is formed by bacteria in the intestines and is stored in the liver. It’s also in foods like green leafy vegetables, fruits, nuts, seeds, whole grains, legumes, and eggs. Folic acid levels in the blood can increase with vitamin B12 deficiency. | Bacterial overgrowth, dietary excess, vitamin B12 deficiency. | Dietary insufficiency, malabsorption, pregnancy, hypothyroidism, megaloblastic anemia, liver disease, celiac disease, vitamin B6 deficiency, carcinomas, inflammatory bowel diseases, anticonvulsant Rx, antimalarial Rx, antacid Rx, birth control Rx. |
| Calcium and phosphorus | Two elements tightly regulated in the body by the parathyroid gland, kidney and vitamin D. Measures can be abnormal with blood and bone disease, kidney disease, hormonal imbalances, intestinal disorders, excessive intake of vitamin C. | ||
| Sodium | An electrolyte necessary for fluid balance and cellular activity. Regulated by kidneys and adrenal glands. | Dehydration. | Vomiting, diarrhea, sweating, fluid overload disorders. |
| Potassium | Electrolyte important for muscles. Very low and very high levels are associated with heart rhythm abnormalities. | Kidney failure, excessive intake of high potassium foods/supplements. | Fluid loss from medications (diuretics), diarrhea, vomiting. |
| Chloride | Electrolyte regulated by the kidneys and adrenal glands. A high or low level usually corresponds to a high or low level of sodium or potassium. | ||
| Iron | This mineral is necessary for red blood cells and is the basis of hemoglobin. Iron can be lost through the intestinal and urinary tract, and through the menstrual cycle. Lost iron must be replaced in the diet. Iron losses in men and post-menopausal women are very low. All iron blood test results can be altered by alcohol consumption, estrogens, birth control, antibiotics, aspirin, and testosterone. Levels also change with the time of day. | Hemolytic anemia, iron poisoning, iron overload syndromes, hemochromatosis, transfusions, excessive supplementations, liver damage, vitamin B6 deficiency, lead poisoning, leukemia, nephritis. | Iron deficiency anemia, blood loss, infections, pregnancy, progesterone birth control pills, pernicious anemia remission, inadequate iron absorption, menstruation, dietary insufficiency, chronic inflammatory diseases. |
| Transferrin | A transport protein largely synthesized by the liver that regulates iron absorption. | Iron deficiency anemia, pregnancy, estrogen therapy. | Microcytic anemia, protein deficiency, infection, liver disease, renal disease, iron overload. |
| Total Iron Binding Capacity (TIBC) | Correlates with transferrin. And iron test without TIBC and transferrin is of limited value. | Iron deficiency, pregnancy, blood loss, hepatitis. | Protein deficiency, hemochromatosis, non-iron-deficiency anemia, liver cirrhosis, renal diseases, hyperthyroidism. |
| Ferritin | Reflects body iron stores and is the most reliable indicator of total body iron status (other than testing bone marrow). May also be a marker of inflammation if elevated. | Iron overload, iron supplements, inflammatory disease, liver disease, leukemia, hyperthyroidism, renal diseases, age, meat consumption. | Iron deficiency anemia. |
| Carbon dioxide | This reflects the acid status of blood. | Lung disease, Cushing’s syndrome, Conn’s syndrome. | Increased acidity from uncontrolled diabetes, kidney disease, metabolic disorders, chronic hyperventilation, Addison’s disease, diarrhea, aspirin overdose. |
White blood cell tests
| Test | What it is | Higher with | Lower with |
| White blood cells (WBC) | These come in many different shapes and sizes. They have a role in the immune response. When the body is damaged, they increase. WBCs produce, transport, and distribute antibodies as well. Alone, a WBC count doesn’t tell you much. | Acute infection, leukemia, tissue injury, malignant neoplasms, uremia, drug use, hemorrhage, post-splenectomy, polycythemia vera, tissue necrosis, steroid therapy (ACTH), afternoon/evening hours. | Viral infections, bacterial infections, hypersplenism, bone marrow depression, bone marrow disorders, pernicious anemia, AM hours, improper blood draw (hemoconcentration). |
| Neutrophils | The most abundant white blood cells that destroy bacteria in the body. | Bacterial infection, inflammation, metabolic intoxications, drugs, hemorrhage, hemolytic anemia, myeloproliferative disease, malignant neoplasms, stress, labor, menstruation, steroid use. | Stem cell disorder, infections, drug use, anemia, chemotherapy, some drugs, temperature changes. |
| Basophils | Involved in parasitic infections and some allergic disorders. | Leukemia, Hodgkin’s disease, myeloproliferative disorders, hypothyroidism, flu, polycythemia vera, hemolytic anemia. | Infection, hyperthyroidism, stress, steroids, chemotherapy, radiation. |
| Eosinophils | Usually involved with allergic disorders and parasitic infections. | Allergies, asthma, tapeworm, endocrine disorders, myeloproliferative disorders, infections, skin diseases, GI diseases, aspirin sensitivity, poisons, stress, PM hours. | Cushing’s syndrome, drugs, infections, AM hours. |
| Lymphocytes | Involved with viral infections like measles, chickenpox and mononucleosis. | Leukemia, mononucleosis, viral diseases, tuberculosis, Crohn’s disease, Addison’s disease, thyrotoxicosis, African-American race, exercise, stress, menstruation. | Chemotherapy, radiation, steroid treatment, aplastic anemia, malignancies, immune disorders, tuberculosis, renal failure, heart failure. |
| Monocytes | Help to combat severe infections. | Bacterial infection, tuberculosis, syphilis, leukemia, certain carcinomas, lymphomas, Gaucher’s disease, trauma, ulcerative colitis, sprue, certain poisons. | Prednisone, hairy cell leukemia, HIV, bone marrow injury. |
Red blood cell tests
| Test | What it is | Higher with | Lower with |
| Red blood cells | These are the most common cells found in blood. They carry oxygen from the lungs to body cells and transfer carbon dioxide from the cells to the lungs. They lack a nucleus, which allows more room to store hemoglobin, the oxygen binding protein.Anemia is a condition in which there is a reduction of circulating red blood cells, the amount of hemoglobin, or the volume of packed cells (hematocrit). | Polycythemia vera, renal disease, tumors, high altitude, cardiovascular disease and dehydration, pregnancy, some drugs. | Anemia, lymphomas, myeloproliferative disorders, hemorrhage, Addison’s disease, infections, recumbent positioning during blood draw, advanced age. |
| Hemoglobin | Gives red blood cells their color. Necessary for transferring oxygen and carbon dioxide. | Polycythemia vera, heart failure, COPD, pregnancy, recent blood transfusions, changes in fluid intake, high altitude, lots of exercise. | Anemia (iron deficiency, pernicious, etc.), liver disease, hypothyroidism, hemorrhage, reactions to drugs, smoking, various illnesses. |
| Hematocrit | The percentage of red blood cells in relation to total blood volume. | Erythrocytosis, polycythemia vera, shock, altitude, pregnancy, dehydration. | Anemia, leukemia, lymphoma, adrenal insufficiency, blood loss, hemolytic reactions. |
| Mean corpuscular volume (MCV) | Determines cell size and can help to classify anemia. Microcytic anemias are usually due to disorders of iron metabolism, heme synthesis, and globin synthesis. Macrocytic anemias are usually due to vitamin B12 or folate deficiency. | ||
| Mean corpuscular hemoglobin concentration (MCHC) | Measures average concentration of hemoglobin in red blood cells. Helps with monitoring therapy for anemia. | Spherocytosis. | Iron deficiency, blood loss. |
| Mean corpuscular hemoglobin (MCH) | Measures average weight of hemoglobin per red blood cell. Helps to diagnose severely anemic patients. High blood lipids and high WBC counts can falsely elevate MCH. | ||
| Red cell size distribution width (RDW) | Indicates the degree of red blood cell size variations. This test is of no value if you don’t have anemia. This test can be altered with alcohol consumption. | Iron deficiency, vitamin B12 deficiency, folate deficiency. | Not significant. |
| Platelets | These are the smallest of the formed elements in blood. They help to stop bleeding by forming clots and assist in vessel integrity. A mean platelet volume (MPV) can help determine bleeding disorders. | Leukemia, polycythemia vera, splenectomy, iron deficiency anemia, asphyxiation, rheumatoid arthritis, infections, lymphomas, inflammatory bowel disease, renal failure, altitude, exercise, birth control medications, winter, lots of excitement. | Pernicious anemia, blood transfusions, infections, heart failure, thrombopoietin deficiency, chemotherapy, HIV, alcohol, renal insufficiency, before menstruation, pregnancy. |
Miscellaneous tests
| Test | What it is | Higher with | Lower with |
| Cortisol | A glucocorticosteroid of the adrenal cortex that influences metabolism of proteins, fats, and carbs. | AM hours, hyperthyroidism, stress, carcinoma, Cushing’s syndrome, adrenal adenoma, obesity, pregnancy, certain drugs. | Adrenal hyperplasia, Addison’s disease, pituitary destruction, hypothyroidism. |
| LDH | An enzyme found in many organs and tissues. When cells are growing or membranes are damaged, this enzyme can leak into circulation. Anything that damages the blood sample can increase this value (including improper handling of the blood specimen). Monitored after a heart attack. | Growing/healing tissues, cellular damage, anemia, liver disease, myocardial or pulmonary infarction, some drugs, exercise, skin disease, alcohol use, stroke, kidney disease, liver disease. | Not significant – sometimes noticed with high supplemental doses of vitamin C. |
| Uric acid | End product of purine metabolism. Transported by plasma from liver to kidney, then filtered and mostly excreted (70% of it). What remains goes to GI tract and is degraded. | Gout, kidney disease, alcoholism, down syndrome, lead poisoning, leukemia, lymphomas, weight loss, metabolic acidosis, liver disease, obesity, altered thyroid/parathyroid function, psoriasis, glycogen storage disease, high animal protein diet. | Fanconi’s syndrome, Wilson’s Disease, SIADH, xanthinuria. |
Mishaps with blood draws
- If blood is drawn from your arm after the tourniquet is on for several minutes, values can be skewed because cells will concentrate in the lower arm.
- If the needle used is too small, it can cause red blood cells to break, leading to a skewed analysis.
- If the puncture site isn’t sanitized – infection can result.
- If you tense up excessively during a blood draw, you can experience extensive bruising at the site.
Summary and recommendations
Getting annual blood work with a physician is a good idea for preventative health. This way you can observe trends and catch potential health problems before they spiral out of control.
Note: If you want to track your health trends over time, make sure to request a copy of your lab results and keep them in a file somewhere.
References
Click here to view the information sources referenced in this article.
Eat, move, and live…better.©
The health and fitness world can sometimes be a confusing place. But it doesn't have to be.
Let us help you make sense of it all with this free special report.
In it you'll learn the best eating, exercise, and lifestyle strategies – unique and personal – for you.

Share