Strong bones are crucial to good health, and good nutrition is crucial to strong bones. Find out what you need to protect the health of your skeleton for years to come.
Nutrition strongly affects bone health throughout our lives. For instance, what our mothers eat while pregnant with us will affect our eventual bone mass as adults.
As children, our bones are almost exploding with rapid growth. If we break something, no problem — we knit back together like Plastic Man. (Which is good, considering how many times we’ll probably fall face-first off the monkey bars.)
By around 18 or 19 years old, we’ve reached about 95% of our peak bone mass. We can continue to build some bone in our 20s.
But by age 30, we stop making any more “bone deposits”. Then the withdrawals start.
This leads me to some bad news and some good news.
The bad news: You’ll lose bone density
Most people in the U.S. lose about 0.5% of bone mass each year after the age of forty. Chronic bone loss leads to low bone mineral density and the deterioration of bone tissue – otherwise known as osteoporosis.
It gets worse.
Fractures from osteoporosis are more common than heart attack, stroke, and breast cancer combined. At least one in three women and one in five men will suffer an osteoporotic fracture during their lifetime.
Osteoporosis is often known as the “silent thief” because the disease proceeds without symptoms.
Many older adults are not aware that they have weak bones until they happen to fall. Women typically lose bone mass drastically during menopause, when bone-protecting hormone levels drop.
And if you’re elderly and you fracture a bone, your chance of dying shortly afterwards skyrockets.
The good news: You aren’t doomed
Luckily, there is a lot you can do even as an adult to protect and even strengthen your bones.
If you understand how bones work, then you’ll understand how you can use good nutrition to keep them strong, solid, and healthy.
What is bone made of?
Bones may look hard and unchangeable. They don’t seem to do anything much.
But like any part of the body, they’re dynamic, living tissues. They’re constantly breaking down and remodeling themselves. In fact, you end up with a completely new skeleton about every 10 years.
And bones aren’t just hunks of minerals, either. Much of the bone structure is actually protein, and contains connective tissues (such as the endosteum or periosteum), a network of nerves and blood vessels, and of course the marrow at the center.
Thus, good nutrition doesn’t just support bone mineralization — it helps the whole skeletal complex stay healthy too.
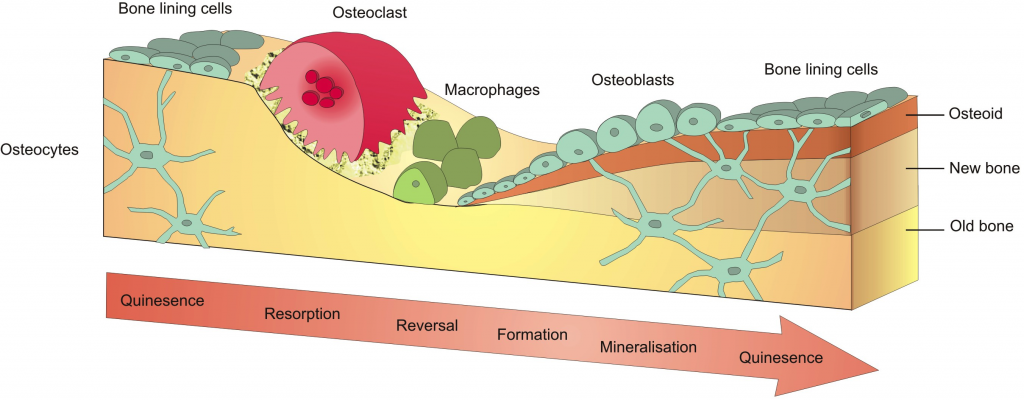
Bone remodeling
When bone cells sense any strain (for example, the impact of striking your foot on pavement as you run, or bearing the load of a barbell), the body sends signals to increase bone formation.
Good nutrition, good remodeling
If we’re well-nourished, then our bones remodel themselves robustly.
Imagine a well-trained construction team renovating a house with high-quality materials.
Microtrauma — tiny cracks and damage — tell the bones to adapt, repair, and ultimately strengthen. Old bone is removed and new bone is laid down. All is well.
If we aren’t well-nourished, then our bones don’t recover well.
Imagine the same construction crew — but this time, their materials are cheap and poor quality. They don’t have the items they need. Maybe they cut a few corners just to get the job done.
The resulting structure is shoddy. New bone isn’t laid down. The old bone just gets weaker over time.
Here’s another piece: As this work crew ages, their efficiency declines. Even when they do have the right materials, they work more slowly.
Nutrition for strong bones
At this point, you’re probably wondering what you can eat – or stop eating – to ensure the healthiest bones possible.
Luckily, it’s simple. Eat a balanced diet of whole, fresh foods. Combine that with regular exercise (so that your bones get the signal to remodel). And your bones will support you for years to come.
Here are some specific nutrients that are involved in bone health.
Calcium
Bone contains about 99% of the body’s calcium, and we need calcium to build bones. That’s why health professionals often tell us to make sure we get enough calcium.
Most folks need between 600-1200 mg of dietary calcium daily. Teenagers probably need the most to support their growth spurts.
Here are some things to keep in mind about calcium:
- Does your body know it should use that calcium? Though calcium is important, it’s not enough to build a strong skeleton on its own. It needs hormonal signals (such as enough vitamin D) and mechanical signals (like impact and loading) to tell it where to go.
- Can your body absorb that form of calcium? We can eat plenty, but our bodies have to be able to use that calcium.
- Is that calcium in balance with other nutrients? Recent evidence suggests that we don’t benefit from supplementing more than 1000 mg of calcium daily — and in excess, supplemental calcium can actually be harmful.
- Are you eating other foods, or taking other medications, that could interfere with calcium absorption? For more on this, see below.

The problem of phytates and oxalates
Many foods contain substances that bind up minerals and prevent us from extracting them.
Two of those substances are phytates (found in grains, seeds, and nuts) and oxalates (found in spinach, rhubarb, sweet potatoes and walnuts).
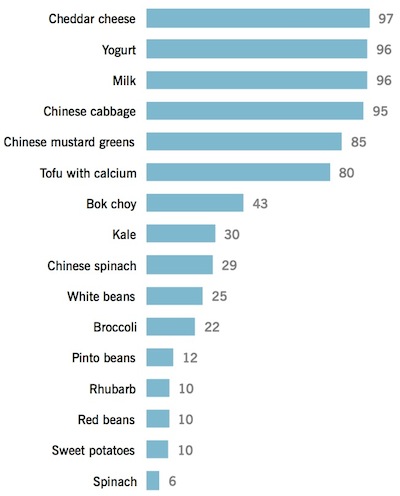
This means that foods like spinach (which contain calcium) are not necessarily good sources of calcium, because the oxalate prevents us from absorbing and using that calcium. However, other foods such as broccoli, bok choy, and kale are happy to help out.
Here’s a handy chart that shows some of the most bio-available sources of calcium.
What percentage of calcium are you absorbing from these foods?
Vitamin D
The “sunshine vitamin”, Vitamin D, does a lot of good things for our health — particularly our bones.
We need vitamin D to build bones and absorb calcium.
If our blood vitamin D levels are under 30 ng/ml (75 nmol/L), our calcium absorption drops by 10-15%. So shoot for a blood vitamin D between 30-40 ng/ml (75-100 nmol/L). (If you’re unsure, get tested.)
Most people should consider supplementing with vitamin D to ensure that D levels are good. Vitamin D requirements vary greatly depending on geography, sun exposure, and current blood levels.
But deficiency is very common, perhaps especially among those with higher body fat, because of the way that lipids change the liver and skin.
Protein
Protein makes up 20-30% of bone mass. Plus, protein intake can influence growth hormones and growth factors in the body, which indirectly affect bone health.
So obviously, we want to make sure we’re eating enough protein.
Some folks worry that high protein intakes are linked to calcium loss. But calcium losses are not a direct measure of osteoporosis. And higher protein intake also leads to higher calcium absorption. In other words, losses and gains might balance each other out.
In fact, the evidence shows that a high-calcium plus a high-protein diet is optimal for bone health. Thus, look for a variety of plant and animal-based protein sources to cover your bases.
Phosphorus
A protein-rich diet is a phosphorus-rich diet. And too much phosphorus may harm bone health. One reason for this is that excess phosphorus can diminish formation of active vitamin D in the body. And we’ve already seen how important vitamin D is to bone health.
On the other hand, too little phosphorus is also associated with poor bone health. The key – as always – seems to be a balance.
Most people get their dietary phosphorus from foods like meat, milk, cheese, poultry, and processed foods with phosphate-based additives.
Phosphorus from additives seems to be more readily absorbed than the phosphorus from whole foods. Thus, consuming more soft drinks with phosphoric acid probably isn’t the best idea for bone health. Phosphorus from grains, nuts, and seeds isn’t absorbed to the same degree because it’s often in the form of phytic acid (see All About Phytates (Phytic Acid)).
Bottom line? As long as you’re getting other nutrients in balanced amounts from whole foods, phosphorus probably won’t cause any problems.
Vitamins K, C, E
Vitamin D is not the only crucial vitamin to bone health. Vitamins K (notably K2), C, and E also appear to be important.
Vitamin K2 helps to guide calcium where it needs to go. Foods rich in vitamin K2 include dairy, meat, poultry, and natto, a traditional Japanese food made from fermented soybeans.
Vitamin C helps to lay down new bone. Foods rich in vitamin C include vegetables and fruits.
Vitamin E acts as an antioxidant to fight off free radical destruction of bones. Foods rich in vitamin E include nuts, seeds, dark leafy greens, and tomato sauces.
Vitamin A
Too little or too much vitamin A may harm bone health. Consuming retinol (a form of vitamin A) in quantities above 1.5 mg/day might negatively influence bones. Check your supplements and fortified products.
Added vitamin A in dairy may play a role in diminished bone health. Again, check labels.
B Vitamins
B vitamins keep homocysteine in check. Higher levels of homocysteine are associated with more fractures (and overall inflammation).
If a diet contains enough food to support lean mass, and a wide variety of whole foods, you shouldn’t need to supplement most B vitamins for good bone health.
The only notable exception is vitamin B12, which many people benefit from supplementing. If you eat minimal animal products and/or are over the age of fifty, include a vitamin B12 supplement in your diet. (1000 mcg, 2 times per week, sublingual preferred).
Sodium
Consuming sodium beyond what the body needs appears to increase calcium losses. While this doesn’t automatically mean weaker bones, it’s probably something to avoid if you can.
Meanwhile, consuming potassium (which comes from vegetables and fruits) might result in a more favorable potassium-sodium balance in the body and help to preserve bone.
Magnesium
Magnesium helps to lay down bone mass.
Foods rich in magnesium include dark leafy greens, beans, seeds, and nuts.
While in theory, we should be able to get enough magnesium from a whole-foods diet, in practice we’ve found that many of our clients (particularly women of reproductive age) are magnesium-deficient and benefit from supplementation.
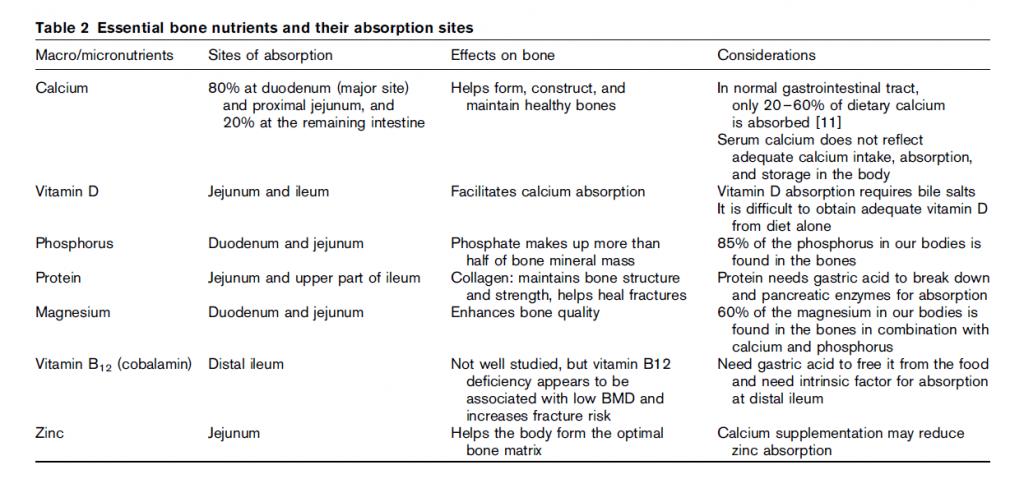
Creatine
Creatine may increase the activity of bone building cells and decrease the activity of cells that break down bone.
But it’s hard to draw conclusions at this point since several studies have also indicated no influence.
Bone-building and bone-busting foods
Knowing the importance of vitamins and minerals to bone health is a great start. But considering your best sources of these vitamins and minerals are whole foods, what should you actually eat for strong bones – and what should you avoid?
Here’s an in-depth look at a few important food groups and their role in bone health.
Vegetables, fruits, beans, whole grains, nuts/seeds
Fruits, vegetables, beans, whole grains, nuts, and seeds all seem to be very beneficial for bones.
This might be due to phytochemicals, specifically flavonoids. Some flavonoids may influence bone cell signaling and prevent oxidation.
One example of the power of flavonoids comes from research involving dried plums. Dried plums (and many dried fruits) are rich in flavonoids. One study indicated that with all else being equal, adding 10 dried plums per day was very beneficial for bone health.
While many flavonoids and other phytochemcials can be identified and isolated, no one really knows yet how many there are. What’s more, their beneficial effects on bone are more likely to come from the way they combine in whole foods than from any particular one.
That’s probably why supplementing with isolated phytochemicals doesn’t appear to have the same protective effects as eating whole fruits and vegetables.
When it comes to beans, soy has been most studied. Its influence on bone health appears to be mixed. Likely, this depends on the way in which it’s eaten. Some of the compounds in soy foods could have a protective effect on bone. But the jury is still out on this one.
Acid/base balance
In addition to their beneficial phytochemicals, vegetables and fruits preserve our bodies’ optimum acid/ base balance, and this, in turn, helps to promote bone health.
There are many mechanisms at work here, but one potential bone benefit for an alkaline diet is that eating more alkaline foods might help to bump up growth hormone levels.
Dairy
Dairy foods are rich in calcium, potassium, and magnesium. This is why they are so frequently recommended as bone boosters. And if you tolerate dairy well, including some in your diet is a good way to ensure you are meeting your calcium needs.
If dairy foods are someone’s lone source of these nutrients, then removing dairy will likely have a negative influence on bone mass. However, if someone gets these nutrients from other sources, then dairy doesn’t appear to offer any additional benefit to bone health.
Fats
Getting a balanced mix of fat sources and types is the best option for controlling inflammation in the body. Controlling inflammation ultimately promotes bone health. I’m aware of no existing evidence indicating that specific fats cause earth-shattering gains or losses in bone mass.
Alcohol
Beer contains silicon, some B vitamins, and polyphenols, all of which might protect bones. Alcohol also has a slight estrogenic effect, which could be bone protective.
However, drinking more than one or two alcoholic drinks per day appears to be problematic for bone health. (And you can pretty much imagine what’ll happen if you try to claim Bud Light as a “bone-building medication” on your health insurance.)
Caffeine
Excessive caffeine appears to be harmful for bones. Up to two cups of coffee a day should not pose risks to someone eating a well-balanced diet.
Mineral waters
Mineral waters might have a favorable influence on bone health, especially if they include calcium or magnesium.
Other dietary factors influencing bone health
Now that you have a better idea of what to eat and why you should eat it, what are some of the other factors that might affect the strength of your bones?
Medications
Medications used in the treatment of depression, breast cancer, heartburn, ulcers, and diabetes can harm bone health, because they interfere with the hormonal signals of bone turnover, and/or because they affect mineral use and absorption.
Other red flags for bone health include prolonged low dose birth control in young women, and prednisone use.
Concern has sometimes been raised about thyroid hormone replacement’s role in bone health. But when TSH is normal, it doesn’t seem to be a risk. That being said, hyperthyroidism is a risk for bone loss, so if you have this, keep on top of your bone density scores.
Dieting and weight loss
Chronic dieters take note: Periods of aggressive weight loss mean that the body isn’t getting enough energy to maintain body mass. Loss of energy often equals loss of mass, including bone.
Bariatric surgeries can result in nutrient deficiencies and weight loss, both of which can result in loss of bone mass.
Exercise may help to offset some of these negative effects and allow people to lose weight safely without compromising bone health. But proper diet is a must.
Disordered eating has a long-lasting negative influence on bone health, likely because of the lack on consistent incoming nutrients and energy.
Eating a balanced diet of whole foods is your best defense.
Body size
Bone health depends on a happy medium — keeping body fat and size within a healthy range (which can vary from person to person).
On the one hand, a bigger body is good.
Higher levels of circulating insulin and weight tugging on the skeleton may stimulate bone growth. With more body fat, leptin levels are usually high, which also helps… up to a point.
On the other hand, if too much of that body size is from body fat, there are problems.
More adipose tissue (outside a healthy range) means more inflammation, which harms (among other things) bone health. Meanwhile, increased fat in bone marrow might be linked to changes in bone formation and a greater likelihood of fracture.
Conversely, a body mass index that is too low — whether excessively lean for too long, or simply under-nourished — also means low bone density.
So, building mass is good, but try to ensure that mass is quality mass — lean muscle and strong, dense bones — rather than freeloading excess adipose.
Conclusions
Bones are actually pretty complicated. But your strategies don’t have to be.
With these simple steps, you can help ensure your skeleton stays strong and springy for life.
- As much as possible, get your nutrients from whole, unprocessed foods, not supplements. Real food is the optimal nutrient delivery system.
- Keep it colorful. Pigment-rich vegetables and fruits deliver vitamins, minerals, phytonutrients and flavonoids — all of which contribute to bone health.
- Check your vitamin D status. If you don’t have adequate levels (30-40 ng/ml or 75-100 nmol/L), supplement until you do.
- Consume several calcium-rich foods each day. This includes dark leafy greens such as broccoli, bok choy, and kale; beans and legumes; dairy; and nuts/seeds.
- Consider a supplement if you really need it, and aren’t getting your calcium from real foods. But avoid using more than 500 mg/day of supplemental calcium. High-dose supplementation won’t help you and is probably harmful.
- Get vitamin K2 (natto, dairy, meat). If you don’t have a regular dietary source of vitamin K2, consider a supplement.
- Drink in moderation. Two alcoholic drinks per day is as party time as it should get.
- Eat some lean protein with each meal. That’s just plain good advice, we think.
- Instead of having cookies or candy when you want something sweet, try dried fruit.
- If you’re trying to lose fat, be sane. Curb your energy intake moderately — not drastically. (May we recommend our PN Coaching program?)
- Maintain a healthy body weight. Being too heavy or too light can negatively influence bone mass.
- Load those bones. Lift weights. Jump. Run. Walk. Carry things. Tell your body you need that bone!
- If you do not eat animal products and/or are over the age of fifty, mix in a vitamin B12 supplement of 1000 mcg, twice a week, sublingual if possible.
- Check your medications, and ask your doctor if adjustments might be useful for long-term bone health.
References
Click here to view the information sources referenced in this article.

Share