Folate deficiency is the most common vitamin deficiency in developed countries, contributing to serious health problems such as neural tube defects (NTD), megaloblastic anemia, digestive disorders, cardiovascular disease, mood disorders, and more. Supplementing with folic acid can reduce the risks associated with folate deficiency.
What are folates?
In 1941, Esmond Snell, one of the 20th century’s foremost biochemists, isolated folates from four tons of spinach leaves. That’s a lot of spinach!
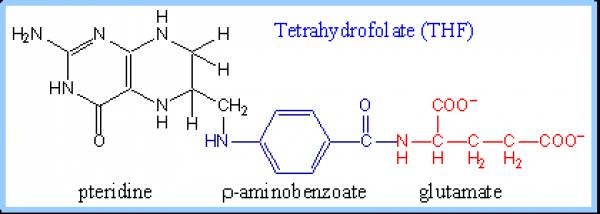
Folates are a group of water soluble compounds that have a chemical structure and nutritional activity similar to folic acid.
Folates and folic acid are sometimes confused. So what’s the difference?
Folates occur naturally in foods. Folic acid is synthesized in a lab and found in supplements and fortified foods. (It rarely occurs naturally in foods.)
Interestingly, folic acid tends to be absorbed better than the folates found in food. This is one case where the “processed” version may actually have an edge over the natural thing!
What do folates do?
Folates help out with many processes in our bodies. They can:
- Improve the efficiency of DNA repair & replication.
- Assist with RNA synthesis.
- Aid amino acid interconversions (including homocysteine conversion).
- Protect us from free radicals and oxidation.
The bottom line is that they help to keep us healthy.
Folates’ role in our health
Folate deficiency
Folate deficiency is the most common vitamin deficiency in developed countries. Deficiency can result from low intake, malabsorption (including Celiac disease and inflammatory bowel diseases) and/or alcoholism.
Folate deficiency can lead to neural tube defects (NTD), slowed growth, megaloblastic anemia, weight loss, digestive disorders, Leukopenia, thrombocytopenia, cracking/redness of tongue/mouth, diarrhea, cancers, cardiovascular disease and behavior changes.
Folates and red blood cells
Red blood cells are produced in bone marrow. Red blood cell production requires a high rate of cell division. Without enough folates, cell division and protein synthesis are limited, resulting in large, abnormal and incomplete red blood cells called megaloblasts. (Hence the disease called megaloblastic anemia.)
However, folates and vitamin B12 are interdependent, and megoblasts can also result from vitamin B12 deficiency. High doses of supplemental folic acid can therefore mask pernicious anemia due to vitamin B12 deficiency.
Folates and pregnancy
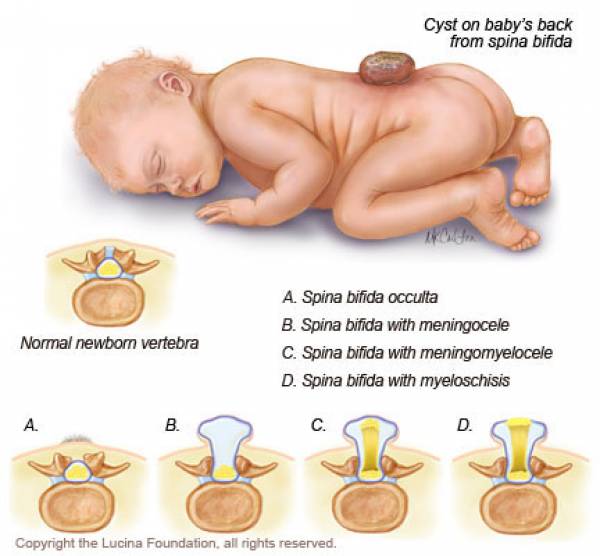
In the 1960s, researchers identified folate deficiency as the main cause of preventable neural tube defects (NTD).
Pregnancy doubles the need for folates. Low folate intake before and during pregnancy can lead to premature birth, low birth weight and NTD.
Supplementing with folic acid before conception can reduce NTD by around 70%. This important discovery led to government recommendations for pregnant women. Since then, food fortification has substantially reduced the incidence of NTD (between 19-49%).
Still, not all cases of NTD can be prevented with supplementation. Plus, high dose folic acid late in pregnancy has been associated with asthma in the fetus.
Since breast milk supplies folates to the infant, mom’s requirements continue to be greater throughout lactation. Breast fed babies tend to have better folate status than formula fed babies.
Folates and cardiovascular disease
Low blood levels of folates are associated with higher blood levels of homocysteine. High levels of homocysteine in the body are associated with cardiovascular disease.
Using a folic acid supplement may not always lower homocysteine levels in the body. But it still appears to be cardioprotective (probably because of the reduction in oxidative damage).
Folates and depression
High levels of homocysteine in the body are associated with depression. Not only that, but higher rates of depression have been found in those who are deficient in folates.
This is probably related to the involvement of folates in the metabolism and synthesis of various neurotransmitters that regulate mood (e.g., dopamine, serotonin).
Folates and cancer
Folates may protect from cancer (particularly colon cancer).
Folates are necessary in methylation reactions. Methylation of DNA appears to be valuable in preventing cancers.
MTHFR (methylene-tetra-hydro-folate-reductase)
MTHFR is an enzyme necessary for homocysteine metabolism. Normal MTHFR is necessary to balance blood levels of folates and homocysteine.
However, some people have a genetic variant of MTHFR that changes its activity, leaving fewer folates and more homocysteine accumulating in the body. Folks with this specific variant likely need to consume more folates.
In mothers with this variant, extremely high levels of homocysteine might occur. This could be a risk factor for giving birth to a child with Down syndrome. At the same time, it’s unclear that supplementation with folic acid can compensate for this. While researchers once believed that mandating folic acid fortification in the U.S. would decrease the incidence of Down syndrome, this doesn’t appear to have happened.
The data aren’t conclusive, but it seems that different genetic variations play a role, along with gene/environment interactions. In other words, at this point, we can’t draw any firm conclusions.
However, many experts suggest that those with genetic MTHFR deficiency (40% of the population carry these genes and 10% express symptoms) supplement with higher dose folic acid or folinic acid (a slightly modified form of folic acid) supplements.
Sources of folates
If someone is eating an adequate and varied diet, it’s assumed they can attain enough folates. Still, folates are unstable and prone to losses during food processing. And folates in animal foods differ due to animal feed, geography and season. Some reports indicate that 30-90% of folates can be lost from farm to plate.
Methods for evaluating folates in food tend to be inconsistent. And bioavailability of folates ranges from 40-70%.
Foods rich in folates include beans, peas, green leafy vegetables, asparagus, organ meat, broccoli, Brussels sprouts, peanuts, tomato juice, banana, papaya and citrus fruit.
Fortification
Food fortification with folic acid was authorized in the U.S. in 1996 and implemented in 1998, providing 140 mcg per 100 grams of food.
Some speculate that fortification isn’t wise – due to some associations between folic acid and subclinical cancers and other poor health outcomes. But these days, to escape all folic acid fortification, you’d have to subsist on 100% unprocessed, unrefined whole foods.
Folates absorption
Most folates are absorbed in the small intestine (the jejunum to be exact). Once folates enter circulation, cellular uptake occurs within minutes.
The body can store about 20-70 mg of folates in the liver. Folates are eliminated from the liver via bile. (While fasting, bile is our main source of folates). They exit the body via urine and feces, usually not as intact folates, but as a breakdown product. Daily turnover is about 90 mcg.
Some foods contain substances that affect folate absorption.
For example, dairy products contain folate binding proteins (FBP). Heat treatment of dairy destroys FBP (and also destroys some of the folates). Fermented milk might contain higher levels of folates (as compared to pasteurized milk). The whey portion of dairy contains most of the FBP. Thus, cheese tends to contain less FBP because much of the whey is separated out during processing.
FBP may act in the mammary gland to trap folates from blood plasma into the milk. It may also assist in the digestion of folates, acting as a sort of intestinal usher, preventing bacteria from consuming the folates.
Catechins and polyphenols (found in tea, cocoa, wine, and other plant foods) can hinder the activity of folates. Daily tea consumption in China has been associated with a higher risk of NTD.
The Dietary Folate Equivalent (DFE) was developed to account for the differences in absorption between synthetic folic acid and naturally occurring folates.
Folates status
The primary indicator of long-term (~100 days) folates status is the red blood cell folates concentration. This measure won’t indicate an emergent deficiency. This test does not require an overnight fast.
Simply measuring the blood level of folates can’t reliably indicate long-term folate status. However, measuring the blood level of folates after an overnight fast can help to pinpoint an emerging deficiency.
High levels of blood homocysteine can also give an early indication of folates deficiency.
If liver stores of folates are full and no additional folates are coming in, signs of deficiency will develop in 3-6 months. The first deficiency signs include megaloblastic anemia, depression, insomnia, cognitive dysfunction, dementia, and mood changes.
Those who abuse alcohol are at risk for folates deficiency.
Summary and recommendations
With modern food processing, it takes a focused effort to meet our intake requirements for folates from food alone.
Most adults should aim to consume around 400 mcg/day DFE (or 240 mcg/day folic acid). To ensure you’re getting enough, feel free to use a supplement. If you want to meet your needs from food, check out the USDA nutrient database and add up what you consume.
The following populations will likely need to increase consumption of folates and/or folic acid/folinic acid supplements:
- Anyone with malabsorption illness (inflammatory bowel diseases, celiac disease, etc.).
- Those with the MTHFR variant (talk to your doc).
- Women who might get pregnant (consume at least 600 mcg of folic acid per day).
- Lactating women (consume 600 mcg per day. Use a supplement to meet these goals.)
- Anyone with elevated levels of blood homocysteine. To control homocysteine, aim to consume at least 400 mcg of folic acid per day. Use a supplement to meet these intake goals. Also, get enough vitamin B12 and vitamin B6. Work with your doc to get blood levels tested.
Toxicity isn’t a concern unless you’re eating lots of fortified foods along with folic acid supplements. Avoid consuming more than 1000 mcg/day of supplemental folic acid (or folic acid from fortified foods).
Extra credit
- Methotrexate is a medication used for rheumatoid arthritis, psoriasis and certain cancers. It’s an antagonist to folates.
- Why might you want to antagonize folates? Well, since folates influence DNA and RNA, they can also influence disease progression. This can be both positive and negative.
- The medication sulfasalazine interferes with folates absorption.
- NSAIDs (non-steroidal anti-inflammatory drugs, e.g. Ibuprofen, Aspirin) can alter the activity of folates.
- Some anticonvulsant medications can decrease the uptake of folates in the body.
- Folates play a role in the bioavailability of nitric oxide.
- Smoking tobacco can inactivate folates.
- Certain strains of probiotics can produce folates.
- Northern China tends to have few vegetables rich in folates. Interventions with folic acid supplementation in this region have shown substantial benefits.
- Low levels of maternal vitamin B12 are associated with a greater risk of NTD.
- Betaine might also help to lower blood homocysteine levels.
- Bioavailability of folic acid from tablets and softgel capsules appears to be similar.
References
Click here to view the information sources referenced in this article.
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.
Share