There are three things related to nutrition and lifestyle that I never want to experience:
- A cardiac catheterization
- A Cinnamon Toast Crunch-induced coma
- A kidney stone
Needless to say, I was excited to write this article.
What are kidney stones?
Kidneys make clean blood by eliminating wastes.
For instance, if you eat a can of soup with lots of salt, the kidney will excrete more salt to balance out levels in the body. If you eat a big steak, more urea will be excreted in the urine.
If the body is unable to eliminate these wastes, you get sick. (Here’s a primer on the urinary system.)
Our kidneys eliminate waste products through urine, and when there is excessive waste or not enough fluid volume, urine becomes supersaturated and a stone can form. Stones can be tiny like a grain of sand or big like a golf ball.

Stones can hang out in the kidneys for years without obstructing any tubing. But when a stone obstructs the ureter, serious pain follows (it’s been said that kidney stones are the worst pain imaginable). The pain can stop/start as the stone heads to the bladder. The bladder tunnel is where most stones get hung up. Since stones may have sharp edges, they can draw blood into the urine.
Kidney stone types
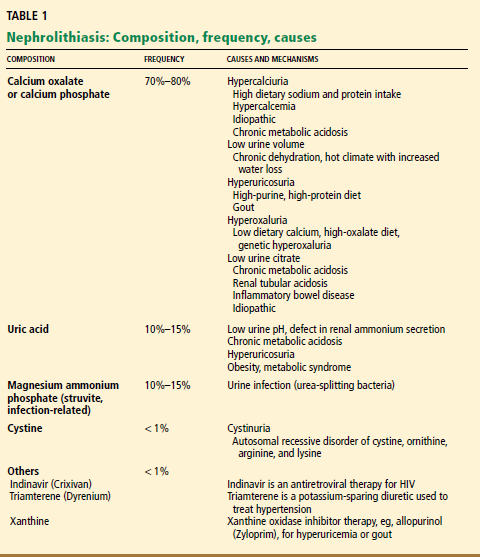
There are four main types of kidney stones:
- Calcium-containing stones – these make up a majority, nearly 75% of stones
- Uric acid stones – these make up about 10% of stones
- Struvite (infected) stones – these make up about 10% of stones and form after an infection in the urinary tract
- Cystine stones – these are stones that form from the amino acid cystine, the most uncommon
The table below shows the composition, frequency, and causes of kidney stones, aka nephrolithiasis (nephro = kidney; lith = stone).
Why are kidney stones important?
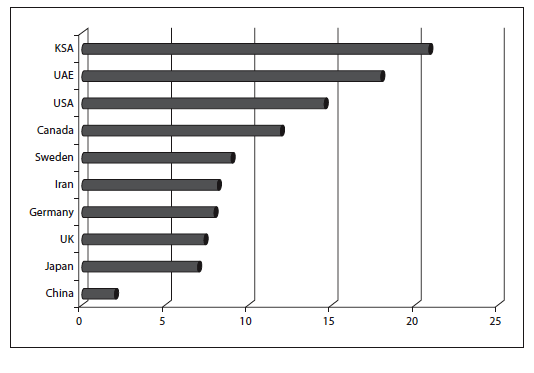
Kidney stones are increasingly common, especially in industrialized and more affluent countries.
By 70 years of age, about 11% of American men and 6% of American women will have had a symptomatic kidney stone. The incidence of kidney stones in the U.S. jumped by nearly 35% between 1980 and 1994 (side note: this increase parallels the rise in obesity).
Kidney stones and chronic diseases
| Throughout the U.S. kidney stones are more common in the summer.This might be due to more sweating (which creates more concentrated urine), more oxalates from fresh fruits and vegetables, animal-protein-heavy barbecues, or all of the above.In fact, a group of researchers predict that climate change, which brings increasingly higher temperatures, will result in more people suffering from kidney stones. |
Several factors seem to affect people’s risk of kidney stones.
For one thing, kidney stones can be a sign of other diseases. Most stone formers also have things like:
- lipid abnormalities
- cardiovascular disease
- type 2 diabetes
- high blood pressure
- excess body fat
- gout
High blood pressure in particular doubles the risk of stones, since it changes how calcium is absorbed in the kidneys.
Diet and kidney stones
Doctors think that people who form stones lack specific chemicals in the urine to prevent them. That’s the bad news. The good news is that these folks can modify what they eat/drink to control stone formation. About two-thirds of people can limit stone formation with basic dietary modifications.
The six major dietary factors in kidney stone formation are:
- Hydration
- Animal protein intake
- Calcium
- Oxalate
- Sodium
- Extreme diets
Factor 1: Hydration
Hydration is probably the most studied area relating to kidney stones. It makes sense: getting enough fluid consistently is vital for stone prevention.
Urine is composed of water, salt, urea, oxalate, uric acid, potassium, magnesium, calcium, oxalate, creatinine, and other acids/waste products of metabolism. The composition of urine changes based on what we ingest. If we don’t drink enough water, or eat excessive amounts of rich foods, the urine becomes more concentrated, which can increase the odds of stone formation.
Concentrated urine can result from someone not drinking enough water, sweating a lot, or eating a rich diet (or a combination of all these factors). When you sweat a lot, you are losing fluid by another means, so you’ll urinate less.
In theory, even if your diet was extremely concentrated in rich foods, if your urine was always dilute, you probably wouldn’t form stones (but you may suffer from hyponatremia).
What you drink can also be a factor.
This is because citrate inhibits calcium stones. We make citrate in the kidney when urinary pH is alkaline.
Potassium citrate found in lemons (and other fruits and vegetables) can increase urinary citrate, which can protect against kidney stones. But citric acid, which is added to many soft drinks, doesn’t appear to be protective. Apple juice, grapefruit juice, cranberry juice, and cola drinks seem to increase the risk of forming stones. Fruit-flavoured soft drinks don’t seem to have this negative effect (including drinks like Gatorade). Naturally carbonated mineral water acquires carbonation from dissolved limestone and can contribute to kidney stone formation.
Thus, water and liquid from whole foods (such as lemons) is ideal.
You should get a minimum of 2 litres of liquid per day (either from water or in foods) to produce adequate urine volume (you want about 2 litres of urine volume). Hydration needs fluctuate with body size, climate, physical activity, etc. — if you’re bigger, warmer, and/or working harder, you’ll want more fluid.
Factor 2: Animal protein
Beyond hydration, a high animal protein intake is probably the most important factor influencing kidney stone development. Why? A few reasons:
- Animal protein contains purines (well, some plant foods do too, but it appears that purines from plants don’t seem to have the same effects in the body). We break down purines into uric acid. Some of this in the body is fine, but too much can supersaturate the urine and lead to stones (both uric acid and calcium-containing types).
- Animal protein makes the urine more acidic, leading to less solubility for uric acid, and suppression of citrate formation. If you don’t consume enough alkaline-forming fruits and veggies, this means trouble.
- Animal protein contains high amounts of glycine and methionine. Glycine is metabolized into oxalate, and methionine can increase urinary calcium.
Data has indicated that those who eat a plant-based diet tend to have a lower incidence of kidney stones, even when including more oxalate-rich plants. Plant-based eaters form stones at about 1/3 the rate of those eating an omnivorous diet. This may be due to the higher intake of citrate-rich foods on a plant-based diet, which can make the urine more alkaline (and help prevent stone formation).
One study demonstrated a 33% increased risk of kidney stones with a 77 gram versus a 50 gram animal protein diet (some people eat this much animal protein per meal). Another trial showed that a diet low in animal protein (52 g/day), sodium (50 mmol/day), and oxalate (200 mg/day), with normal calcium intake (1200 mg/day) was associated with a reduction in stone formation of almost 50% over a five year period.
It’s important not to restrict protein below 0.8 g/kg body weight per day (so, for someone who weighs 180 pounds, this would be about 65 grams of protein per day), as this can increase parathyroid hormone and calcium in the urine.
For more on acid-base balance, see All About Dietary Acids and Bases.
Factor 3: Calcium
When we consume and absorb high levels of calcium, we must excrete the excess. One way to excrete calcium is via urine. Higher levels of calcium in the urine can increase the chances of kidney stones for certain individuals (calcium is the most abundant mineral in kidney stones).
While excessive calcium intake isn’t a good idea, a low calcium diet might be even worse.
First, not getting enough calcium can harm bone health.
Second, eating calcium rich foods can help bind oxalates in the gut (see below for more on oxalates) and get rid of them in the stool (before they’re absorbed and travel to the kidneys).
Finally, a low calcium intake leads to bone breakdown and higher levels of calcium in the urine.
What about calcium supplements?
Well, when calcium isn’t bound to natural co-factors in food, the delivery system is altered, and the calcium may end up in places we don’t want (e.g., calcification in vessels and kidneys). Further, the body might attempt to relieve itself of the elemental calcium by pushing it through the kidneys (resulting in stones).
If you supplement with calcium, balance your intake with foods, only use calcium citrate, make sure vitamin D status is controlled (not too high or too low), and consume supplements with meals.
About 800 – 1000 mg per day of calcium should be plenty (total – from food and supplements).
Factor 4: Oxalates
Oxalic acid is a naturally occurring substance that can bind with minerals. Oxalates are kind of boring, well, until they crystallize with calcium to form kidney stones.
When someone has lots of oxalates in their urine, where the heck did they come from? Well, there are five potential sources of oxalates:
- Oxalate-rich plant foods
- Waste products of general metabolism
- Vitamin C supplements
- Animal protein
- Beverages
Source #1: Oxalate-rich plant foods
Oxalate content in plants can vary because of differences in climate, soil, ripeness, or section of the plant analyzed. Younger plants have more oxalic acid, which we absorb more of. Older plants have formed calcium oxalate salts, which we absorb less of.
Foods higher in oxalates include:
- spinach
- rhubarb (the leaves are so high in oxalates they are poisonous)
- beets
- amaranth
- Swiss chard
- chives
- parsley
- cocoa
- berries
- bran
- nuts
Panicked yet? Don’t worry — dietary variety is your friend.
Swap out kale for spinach. Don’t eat rhubarb leaves. Only eat beets during the peak season. Lots of cocoa means lots of chocolate, and if you are consuming it regularly, you’ll have problems beyond kidney stones. Incorporate pumpkin seeds, sunflower seeds, flax seeds, and macadamia nuts in place of higher oxalate nuts/nut butters.
Seasonal eating can help control oxalate intake. Some people eat spinach and berries year round. Holy oxalates. Instead, each spinach and berries only during peak seasons. During the other months, switch to lower-oxalate foods like cauliflower and apples.
A “normal” day of eating might include 80-100 mg of oxalate/day, and we only absorb about 10-20% of that.
After oxalates are absorbed, the only way to get rid of them is in the urine.
Excreting excessive amounts of oxalates in the urine is called hyperoxaluria, and it’s unlikely that you’ll end up with that from dietary intake alone. Rather, it’s from overabsorption in the gut (more oxalates are absorbed in the gut when someone is suffering from inflammatory bowel disease), low dietary calcium intake (remember, calcium binds oxalates in the gut), low fibre intake, and endogenous production.
Oxalates from food are tricky. Some data even indicates no added risk for stone development from oxalate-rich food.
Source #2: Waste products of general metabolism
Normal metabolic processes in the body contribute to oxalate formation.
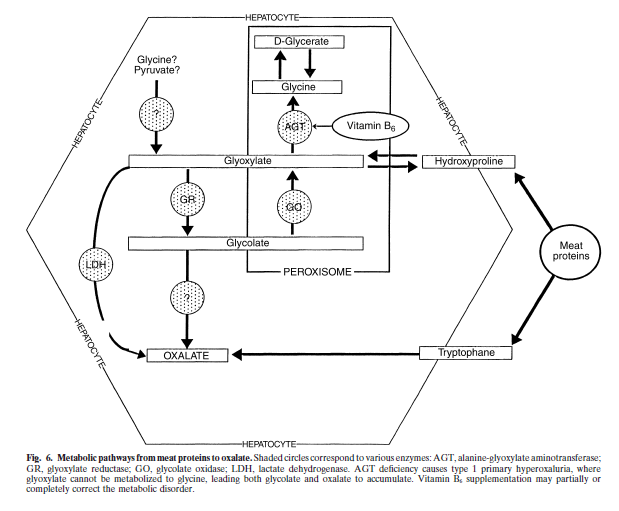
Vitamin B6 (pyridoxine) is a cofactor in the conversion of glyoxylate to glycine, and its deficiency could increase oxalate production in the body. So get enough vitamin B6 from sources like whole wheat, brown rice, green leafy vegetables, sunflower seeds, potato, garbanzo beans, banana, spinach, tomatoes, avocado, walnuts, peanut butter, lima beans, and bell peppers.
Source #3: Vitamin C supplements
Vitamin C supplements (ascorbic acid) can be metabolized to oxalic acid once ingested.
Source #4: Animal protein
When we use amino acids as an energy source, oxalate synthesis can result. Also, data indicates that a precursor to oxalate, called glycolate, might increase as we consume more animal protein. Still, these results are variable based on what type of stones the person tends to form.
Source: Nguyen QV, et al. Sensitivity to meat protein intake and hyperoxaluria in idiopathic calcium stone formers. Kidney Int 2001;59:2273-2281.
Source #5: Beverages
Cola soft drinks may lead to higher levels of oxalates in urine, while decreasing magnesium and citrate. Bad news if you like your kidneys. Still, some data indicates that caffeine and sugar-free colas don’t have any negative influence on stone formation.
Those who drink small amounts of coffee, alcohol, and tea may have a lower risk of kidney stones, even though these beverages can contain oxalates. Drinking coffee/tea with milk can further bind oxalates and prevent absorption (this is due to calcium, so any non-dairy milk fortified with calcium would work). Green teas, rooibos teas, and herbal teas tend to contain less oxalate than black teas.
Excessive sugar consumption (from food or drink) may lead to increased oxalate, calcium, and uric acid in the urine.
Factor 5: Sodium
As we increase sodium in the diet, urinary calcium excretion increases, and this can influence stone formation.
By now, most everyone knows (I hope) that we get most of our sodium from processed foods. Limiting sodium to less than 2300 mg per day — simply by switching to unprocessed, whole foods — can greatly decrease the amount of oxalate and calcium in the urine, both extremely helpful in preventing stones.
A note on sodium: if small amounts of sodium in a beverage help someone keep fluid intake at 2 litres per day, the benefits of more fluid outweigh the risks of more sodium.
Factor 6: Extreme diets
We know that yo-yo diets are a great way to form gallstones, but risk for kidney stones also goes up.
Large meals and binge eating, especially at night before sleep, can lead to very concentrated urine. Further, with yo-yo dieting we repeatedly break down stored body fat for energy, leading to metabolic by-products (including ketones) that must filter through the kidneys. These by-products tend to make the urine more acidic, which can lead to stones.
Lower-carb, higher-fat/protein diets can increase urinary acidity, lower urinary citrate, and raise urinary calcium – increasing the chances of kidney stone formation.
Factors beyond our control
Genetics
Kidney stones tend to run in families. If you have a relative with kidney stones, your risk is 2-3 times higher of getting one. Specific factors have been associated with this.
Alanine:glyoxylate aminotransferase (AGT) is a vitamin B6 (pyridoxine) dependent enzyme found in the liver that converts glyoxylate to glycine, reducing the formation of oxalate from glyoxylate.
A genetic variation can result in more AGT in the mitochondria rather than perioxisomes. Peroxisomes deal more effectively with plant-derived glycolate, whereas mitochondria handle meat-derived hydroxyproline – both sources of glyoxylate production.
Thus, certain AGT genetic variations may affect a person’s response to their diet — and affect whether a plant- or meat-based diet works better. (This may also explain why researchers are still figuring out which dietary factors are most relevant: people may differ in their genetic risk and dietary response.)
Other genetic variations may directly influence oxalate absorption in the gut and sodium-phosphate transporters in the kidney.
Chronic diseases and health problems
There are various medical conditions that can lead to kidney stone formation. These conditions include:
- Bowel disease
- Medullary sponge kidney
- Hyperparathyroidism
- Milk-Alkali syndrome and ulcers – this increased in the early 1900s when folks tried to control ulcers with milk and antacids, leading to dangerous levels of calcium in the blood. This condition is on the rise again due to increased use of calcium and vitamin D supplements.
- Anatomic abnormalities with the kidney
- Paralysis
- Renal tubular acidosis
- Cystinuria
- Oxalosis
Medications used to treat kidney stones include:
- Alkaline potassium salts – used to raise urinary pH. You may need to dilute them with water if they cause stomach upset.
- Alkaline sodium salts – an alternative to potassium salts.
- Thiazides – diuretics used to decrease urinary calcium. You must control sodium intake when using them. They can deplete potassium levels in the body.
- Allopurinol – reduces production of uric acid in the body. Extremely serious side effects.
Summary and recommendations
We’ve made a lot of advances in our medical treatment of kidney stones. But ideally, you don’t ever want to have a kidney stone — or worse, have more than one.
Here are some ways to lower your risk.
Keep urine dilute
Drink at least 2 litres of water per day. Small amounts of coffee, tea, lemon water, and alcohol may also be helpful.
Get rid of the excess
If it doesn’t use stuff, our body has to excrete anything that we ingest. Overeating, overdrinking, and overmedicating can lead to more work for the kidneys. Big meals, yo-yo dieting, and binging put big demands on the kidneys and can promote stone formation. Avoid big meals before bed. (You’ll sleep better that way anyway.)
Vary fruit, vegetable, and nut/seed intake
If you rely on oxalate-rich foods year round, your kidneys might get overwhelmed. Eat a variety of foods, and eat with the seasons to give your kidneys a break. The food will be fresher, too. Bonus!
Limit animal protein
If you’re at risk, consider lowering your animal protein intake to no more than about 50 grams per day. Make up the rest from plant sources as much as possible.
Limit sodium intake
Less than 100 mmol/day (2300 mg/day). This is easy if you don’t eat processed foods.
Stay lean
Less body fat turnover means fewer waste products for the kidney to deal with.
Control calcium
No more than 800-1000 mg/day of calcium (food and supplements combined). With calcium, you don’t want to go too high or too low.
Use vitamin supplements with caution
Vitamins A and D can lead to increased calcium in the urine and stone formation. Only supplement with vitamin D if you require it (based on blood testing), watch out for fortified foods.
Vitamin C supplements can be excreted in the urine as oxalate. Avoid using them unless you’re deficient.
This includes fortified foods/drinks.
If you have stones, find a specialist
Watch out for internet scams.
Avoid antacids with calcium base
These can cause phosphate depletion and increase calcium in the urine.
Extra credit
Ben Franklin suffered from kidney stones.
Adequate magnesium intake may help to prevent oxalate stone formation in the kidneys. Sources of magnesium apples, apricots, avocadoes, bananas, whole grains, nuts, and green leafy vegetables.
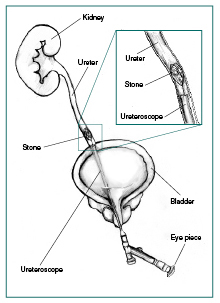
If you don’t care about kidney stones, you will after seeing a picture of a ureteroscopy!
Although kidney stones are generally higher in affluent regions, the highest incidence for kidney stones throughout the world is among uranium workers in eastern Tennessee and adults in northeast Thailand.
The protease inhibitor indinavir, used in HIV/AIDS, can increase risk for stones.
A high fat intake can increase oxalate absorption.
The ratio of calcium to oxalate in urine is usually 10:1.
Stones risk increases with a protein rich diet, but also from malnutrition.
There is currently no analysis or research that shows whether oxalic acid is present in hemp. Living Harvest is hoping to perform analysis by 2011.
NSAIDS and acetaminophen, used chronically, can damage the kidney, and increase odds of stone development.
With pregnancy comes changes in urinary pH, which can increase chances of stone development.
South Africans are virtually resistant to kidney stones, but standard urinary measurements haven’t been able to isolate why.
The drug Flomax might help to increase the likelihood of spontaneous stone passage (in someone with a passable stone).
References
Click here to view the information sources referenced in this article.
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.

Share