In this week’s case study, a man who fears he’s having a heart attack discovers that a few small lifestyle changes can help him eliminate chest pain.
Eat less and exercise more. It’s generally a great prescription for improving health and improving body composition. However, it doesn’t always work.
Even with an awesome exercise plan and a rock-solid diet, some people suffer from mysterious symptoms and complaints that seem puzzling, given how much effort they put into their fitness and health.
When we meet clients who have problems that exercise and nutrition — not to mention their own doctors — can’t seem to solve, we know there are only a few experts on the planet to turn to. One of them is Spencer Nadolsky.
Dr. Nadolsky is a doctor of osteopathic medicine who’s also studied exercise physiology and nutrition. An academic All-American wrestler in university, he’s still an avid exerciser and brilliant physician who practices what he preaches to patients -– treating preventable diseases first with lifestyle modifications (instead of prescription drugs).
When clients have nowhere else to turn, Dr. Nadolsky turns from a cheerful, sporty doctor into a meticulous, take-no-prisoners forensic physiologist. He pulls out his microscope, analyzes blood, saliva, urine, lifestyle – whatever he has to, in order to solve the medical mystery.
When Dr. Nadolsky volunteered to work on a regular case study feature with us, we jumped at the chance. By following along with these fascinating cases, you’ll see exactly how a talented practitioner thinks. You’ll also learn how to improve your own health.
In today’s case, we’ll meet a man with regular bouts of chest pain who goes to the hospital thinking he’s having a heart attack. Thank goodness our Doctor Detective is on the case.
Using the best practices of medicine, lifestyle coaching, and change psychology, our doctor comes up with a strategy to help diagnose the problem. And a program to help get the patient feeling better in less than a month.

The client
Ron, a 52 year old male, came to the hospital for “chest pain”.
While working in the hospital, it’s quite common to see men his age come in for this reason. But while common, the complaint of “chest pain” cannot be taken lightly.
Just looking at Ron as he rested in the emergency room, I worried that he was having a myocardial infarction (heart attack). He had a sedentary look to him that didn’t bode well. But while a patient’s appearance gives clues to his risk for a heart attack, his history is even more important.
The client’s signs and symptoms
Ron’s blood pressure was 152/93, his BMI was 34, and his waist circumference was 42 inches. All were well out of healthy range.
Not good news. I needed to find out more.
After introducing myself, I asked him to describe his pain. Ron said he felt a severe burning behind his sternum that “possibly” radiated to his left arm. He mentioned he’d had similar episodes in the past, particularly after eating, but none this bad. When asked about chest pain during activity such as exercising or even activities of daily living (cooking, cleaning, yard work, etc.) he denied having any.
Next I began to explore his other risk factors for heart attack. Luckily, he didn’t smoke, but he said his dad had a heart attack around the age of 50. As you can imagine, he was pretty scared. As for me, like any good detective, I was recalculating his risks with every question.
| Signs / Symptoms | My thoughts – potential issues |
|---|---|
| Substernal chest pain | Serious: Heart attack, pulmonary embolism, aortic dissection, pneumothorax, esophageal rupture, pancreatitis, sometimes gall bladderNon emergent: Costochondritis, GERD (gastroesophageal reflux disease), esophageal spasm |
| No anginal pain (pain with exertion) | Less likely to have coronary artery disease |
| Pain after eating | More likely to be gastrointestinal related, but cannot rule out heart/lung involvement on this alone |
| Pain radiates to left arm | More indicative of heart involvement but definitely not 100%. |
Based on his symptoms, there was no way of ruling out heart problems. So we needed to run some tests to ensure he wasn’t experiencing a heart attack.
Before beginning with those, I performed a quick physical exam. The results were essentially normal. Ron’s heart was beating at a regular rate and rhythm without any murmurs or gallops, his lungs were clear on both sides, and his belly was soft and non-tender to touch or pressure. All good signs.
The tests and assessments
First and foremost, Ron needed an electrocardiogram (EKG or ECG). ECGs show the electrical activity of the heart. If there is ischemia (decreased blood flow) or an infarction (complete lack of blood flow) in the heart, the electrocardiogram will often pick this up.
Ron’s ECG
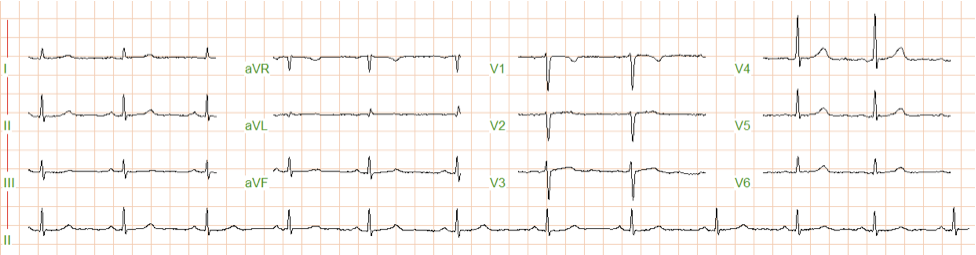
It takes a lot of repetition to learn the patterns of an electrocardiogram as well as to understand the significance of the patterns. To simplify, let me just say that this ECG shows no signs of ischemia or infarction.
While ECGs are a great tool for diagnosing heart attacks, we also have lab tests that show if there has been damage to the heart from a lack of blood flow called cardiac enzymes — specifically, troponin I and creatine kinase MB fraction. Along with the cardiac enzymes, we test for an array of other conditions that could be causing the pain.
The test results
Blood chemistry panel
These are Ron’s pertinent lab findings:
| Marker | Result | Lab Reference Range | Thoughts |
|---|---|---|---|
| Troponin I (x 3 sets every 3 hrs) | <0.02 | <0.04 | No signs of cardiac damage after 3 separate sets. |
| Creatine Kinase MB | 2.0 ng/mL | 0.0-4.5 | No signs of cardiac damage. |
| AST/SGOT | 19 IU/L | 0-37 | No signs of liver inflammation/damage. |
| ALT/SGPT | 23 IU/L | 0-41 | No signs of liver inflammation/damage. |
| Lipase | 13 IU/L | 13-60 | No evidence of pancreatitis. |
| Total bilirubin | 1.0 mg/dL | 0.1-1.5 | Normal. Likely no liver or gall bladder issues. |
| Total cholesterol | 183 mg/dL | 100-199 | Normal. Although the total cholesterol is not a good measure by itself. |
| HDL | 37 mg/dL | >39 | Too low. I would like this to be higher for better cardio-protection. |
| Triglycerides | 156 mg/dL | 0-149 | Higher than I would like. A sign of metabolic syndrome / poor diet and exercise habits |
| LDL | 120 mg/dL | 0-99 | High, but I wouldn’t add a statin right now. |
| Non-HDL | 147 mg/dL | 0-130 | A little high. Possible increased risk of coronary artery disease. |
| Fasting glucose | 100 mg/dL | 65-99 | Ron is teetering on a diagnosis of pre-diabetes. He is probably a little insulin resistant, which doesn’t help his risk. |
As you can see from the above tests, Ron was likely not having a heart attack. As further confirmation, his pain had basically resolved once he relaxed in his not-so-comfy bed in the hospital.
But my job wasn’t finished yet.
First, to assess Ron’s risk for coronary artery disease (narrowing of the blood vessels to the heart), I ordered a stress test. While there are several types of stress test available, Ron performed the exercise version. This test involves walking on a treadmill while hooked up to an ECG. The speed and incline are increased every three minutes until the patient can’t go any longer or there are specific ECG changes related to decreased heart blood flow.
Along with this test, doctors sometimes add an ECHOcardiogram in order to look inside the body and actually see the heart wall and valve function.
Much to Ron’s excitement, he passed the stress test with flying colors, despite his relatively sedentary lifestyle.
The good news: Now we knew that he very probably did not have coronary artery disease. But we still didn’t know what was causing his chest pain.
Ron left the hospital with a diagnosis of atypical chest pain, which basically means not cardiac-related.
But I wanted to follow up in my clinic because, based on his symptoms, I thought I might be able to help him. While his chest pain was not life-threatening, his family history and sedentary lifestyle still put him at some risk for developing heart disease. And the chest pain was making him very uncomfortable! I was determined to decrease his risk factors and fix his chest pain in the bargain.
Ron’s first clinic visit
Though he was relieved to know he hadn’t been having heart attacks, Ron was still dealing with chest pain, and the pain had been coming more frequently lately – especially after dinner.
By this time, I was about 98% positive that Ron was experiencing GERD (gastroesphogal reflux disease). The signs and symptoms fit, and we’d already ruled out heart problems.
Luckily, the habits that protect against future heart problems also alleviate reflux. Bonus!
In most cases, losing weight alone is enough to end GERD. Losing weight would also decrease Ron’s risk of coronary artery disease, improve his insulin sensitivity, and protect him against diabetes.
With all that in mind, my first goal was to ensure that Ron didn’t eat right before bed. Eating shortly before going to bed can increase a person’s chances of experiencing heartburn because of increased stomach acid levels.
I also asked him to increase the angle of his pillow to allow gravity to help him digest. He agreed this was an easy fix.
Finally, I wanted to add a dietary habit for him to practice before his next appointment: No alcohol.
From Ron’s point of view, this was a lot to ask. He didn’t want to give up his nightly 2-3 beers. But after some discussion, he agreed to reduce his drinking to 1 beer, 3 nights a week. A compromise – but one that Ron felt confident he could commit to, which is crucial when we’re asking for lifestyle change.
Ron’s follow-up
Three weeks later, when the nurse handed me Ron’s vitals, I was pleasantly excited to see he had already lost 3 pounds!
Now, this might not seem like much, but considering he had only changed one small habit, 3 pounds is a significant weight change.
Of course, it’s possible that Ron had underreported his earlier drinking; patients often do this. In that case, by cutting down to only three drinks a week, he would also have reduced his calorie intake considerably, and that on its own would explain the weight loss. But either way, he was drinking less, and was seeing some results already.
While I was glad to see Ron’s weight loss, I was even more curious to hear about his chest pain.
Guess what? The pain was down to 2 or 3 nights per week!
As good detectives, you can probably guess which nights he was experiencing pain. Hmmm.
Ron was pleased with these improvements. But he also wanted to know how to reduce his chances of developing diabetes.
I explained that if he continued to lose weight, he probably wouldn’t develop diabetes.
This seemed to be the motivation Ron needed to get more serious about changes to his lifestyle. He asked me about weight loss methods.
So I prescribed a modest program of resistance training. At the same time, I asked him to eat more protein.
I also told him to start supplementing with berberine to increase his insulin sensitivity.
We agreed that in another month, we’d check his glucose and cholesterol for changes.
The prescription
Some doctors might have thrown a proton pump inhibitor or an H2 blocker at Ron to help with his gastroesophageal reflux disease. But drugs don’t get to the root of the problem and I refuse to prescribe them as a first line treatment. Lifestyle changes, if the patient will make them, are always best.
Fix #1 – Sleep position
Raising the head of his bed with some extra pillows allows gravity to do its work and pull Ron’s food into his stomach. If you lie flat, your food can more easily go back up (aka reflux)!
Fix #2 – Weight loss / decreased alcohol consumption
Decreasing alcohol alone can sometimes reduce or even end GERD. In this case, the benefits would be even greater. But cutting down on alcohol, Ron would also lose weight. And his weight was at the root of his problem.
Weight loss isn’t easy – but it isn’t complicated, either. Small changes to dietary habits, along a decent exercise program, will usually result in lower weight.
Fix #3 – Increase insulin sensitivity
In order to accelerate Ron’s weight loss process, I added the insulin sensitizing supplement berberine HCl. Berberine HCI not only helps with weight loss, but it also improves blood sugar and cholesterol issues.
The outcome
Another month later, Ron was free of his chest pain .
He had lost a total of 10 pounds and 3 inches off his waist. His blood pressure was down to 127/81. His fasting glucose was had gone from 100 to 87 mg/dL, his HDL had gone up to 41 mg/dL (vs. 37), triglycerides were well within reference range now at 95 mg/dL, and his LDL was down to 101 mg/dL. Great improvements. Not only that, but he was following his new dietary and exercise habits about 80% of the time.
In a rather short time, Ron had rid himself of the annoying reflux and reduced his risk factors for coronary artery disease and diabetes. Pretty amazing for someone who, not too long ago, had thought he was having a heart attack – and who’d looked as if he might be having one, too!
Take-away
So what can we take away from Ron’s story?
- There are many reasons for chest pain. If you have chest pain and have a feeling it might be serious, get it checked out immediately.
- If you have some chest discomfort after eating (especially at night) it could be GERD.
- GERD can often be resolved with weight loss and elevation of your head after eating. Try not to jump straight to prescription drugs. If lifestyle changes don’t diminish your GERD, further evaluation is in order.
- Weight loss is a very powerful tool to alleviate many chronic conditions, including GERD.
Learn more
Want to get in the best shape of your life, and stay that way for good? Check out the following 5-day body transformation courses.
The best part? They're totally free.
To check out the free courses, just click one of the links below.

Share