Hot flashes, mood swings, weight gain, brain fog: Menopause can make you wonder if your body is totally cuckoo. But what many women don’t realize is that they do have some control over these symptoms. Here’s what’s going on, plus six lifestyle strategies to feel your best during menopause.
- Want to listen instead of read? Download the audio recording here…
++++
Mood swings. Weight gain. Waking up to sweat-soaked pajamas and bedsheets every… darn… night.
Menopause can feel weird, uncomfortable, and downright scary for many women.
Your body is suddenly doing all this stuff you don’t recognize.
Sometimes it feels like your body and brain are no longer under your control.
You ask yourself…
Is this normal?
Is my body against me?
Is there anything I can DO?!
When you look to the internet for advice, you’re confronted with headlines like this:
“8 sneaky symptoms of perimenopause — Do YOU have it?”
“Rare jungle herbs to cool your hot flashes & heat up your libido!”
“Fight biology and battle your meno-belly with this celebrity diet.”
This is not that kind of article.
We won’t prescribe a “to do” list so you can “overcome” menopause.
No “life hacks”, “cool tricks”, or “quick fixes” either.
Instead, we hope to help you:
- understand your body;
- appreciate the intelligent adaptations it makes with age; and
- embrace change, with all the possibilities that come with it.
Because if you’re a woman (or if you coach women), understanding what’s changing during menopause, why it’s happening, and how to deal with it can make the whole process a lot less confusing, uncomfortable, and frustrating.
While you might feel like your body is all over the place, you actually do have control over your mindset, your lifestyle, and your environment — all of which also affect the symptoms that come along with menopause.
You have the power to affect your hormones.
Yep, really.
There are things you can do to ensure you feel healthy, strong, and — yes — sexy during menopause.
- If you’re a woman going through perimenopause or menopause, you might find recognition and relief in this article. You’ll learn exactly what’s going on with your body and what you can do about it.
- If you’re a woman who hasn’t yet reached perimenopause or menopause, you’ll learn about what lies ahead. That way, when it happens, you’ll know (or at least have some ideas about) what to do.
- If you’re a coach who works with women, you’ll gain insight into what your female clients or patients in midlife may be experiencing. Understanding what’s happening on a biological, psychological, and social level will help you sharpen your coaching superpowers.
In this article:
- We’ll outline and examine the different hormonal phases of a woman’s life.
- We’ll explain what causes menopause and its warm-up act, perimenopause.
- We’ll explore how menopause can affect the body, the symptoms women commonly experience, and what can help.
- We’ll suggest lifestyle habits and strategies that can help you feel empowered and in control of your hormones during midlife.
++++
First, a disclaimer.
Of course, not all women will experience what we’re describing.
We’re speaking here about bodies that have female reproductive systems and a hormonal environment that’s within the statistically “normal” range.
But some people with female reproductive systems don’t identify as female.
And just as there is no single standard experience of menopause, there’s also no single standard way to be a woman (or, for that matter, a man).
People are diverse, and that’s a good thing.
Take what’s useful for YOU from this article, and leave the rest.
A woman walks into a medical office…
Yes, menopause often starts like the first line of a bad joke.
It might begin with your period getting a little wonky.
Maybe it starts showing up late (or early). Or it’s longer (or shorter), more painful (or less painful), heavier (or lighter). And sometimes it doesn’t show up at all.
And it’s not just your period.
Whatever your “normal” is starts changing.
Sleep deceives you.
Like a fickle ghost, it visits only at random points in the night.
Your temperature is weird too.
You might find yourself going for a walk in the middle of winter and having to tear your scarf off and unzip your jacket, your neck literally steaming.
You might be a little moodier than usual.
Yesterday at the drugstore, you became enraged because you couldn’t find the toilet paper brand you wanted. I can’t use this sandpaper! you howled at the confused clerk, and stormed out.
Maybe you’ve heard about these symptoms before. From girlfriends, from your older sister, from Googling late at night when you can’t sleep… again.
So you make an appointment with your doctor.
You sit down with your doctor and tell them about your symptoms:
“Hey doc, my vagina is chafing and feels like fire… just kidding… unless you know what to do about that?”
“Hey doc, let’s say someone bled for 17 days last month. Is that normal? I’m asking for, er, a friend.”
“Hey doc, yesterday at the gym, mid-squat, I peed a little. It also happens when I cough, laugh, orgasm, jump, or yell at my dog in a sudden fit of fathomless rage.”
Your doctor tells you these symptoms are consistent with perimenopause.
Wait, what? You’re only 38! You thought hormone stuff was for, like, your mom.
There’s no single start or end point for menopause.
You might look back on one moment in your life as “the time I realized I was a grown-up”.
Holding that first retirement fund receipt. Buying clothes for quality stitching, not style. Keeping an orchid alive for more than 8 weeks.
But biology operates on a continuum. That means there’s no single moment when menopause (or perimenopause) begins.
In general, physiological processes and systems are complex and ever-changing.
They ebb and flow from moment to moment, and year to year.
That means:
Menopause is a dynamic and responsive process, not a single event.
And it may show up when you’re not expecting it.
Just as we go through puberty at different ages, perimenopause and menopause kick in at different times, too. Usually, perimenopause begins in a woman’s 40s (although it can happen as early as her 30s), and menopause can happen anytime between a woman’s 40s and 60s.
The exact timing varies for each woman. It’s is kind of like a repair person who says they’ll be there between 9am and 8pm — a bit hard to predict.
That said, there are some distinct hormonal stages, which generally work as a linear process. Our first major hormonal event is that zit-sprouting, growth-spurting, heart-palpitating time — puberty!
When we hit puberty, our hormonal factories open for business.
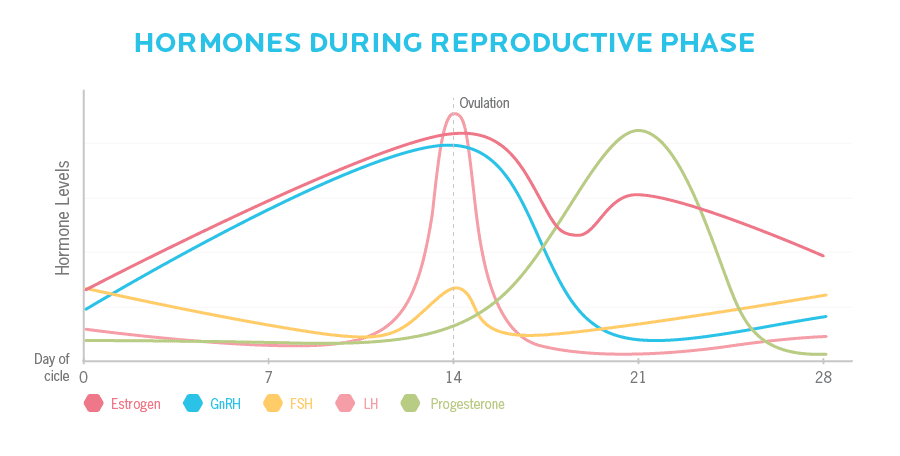
In our reproductive years, a complex symphony of hormonal feedback loops occurs approximately once a month.
Our brain sends a signal to our ovaries, which respond by increasing production of the reproductive hormones estrogen and progesterone and other related hormones. We ovulate, build a uterine lining, shed it, and begin the cycle again.
Over and over, these hormonal feedback loops carefully coordinate to ensure that the uterus can support a fetus.
Hormones are pulsatile (meaning they’re released in bursts), and strongly affected by a variety of factors.
At some point, the feedback loops start to change subtly.
Perimenopause is the time before menopause.
As women age, their ovaries gradually start producing less estrogen, progesterone, and other related hormones.
However, this isn’t a linear or steadily progressive process.
Just like during reproductive cycles in the years prior, hormone levels vary throughout menopause.
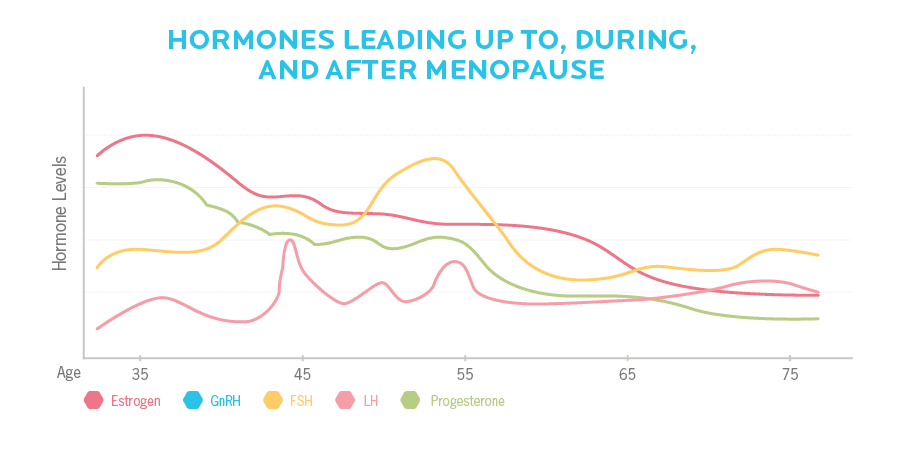
Just like within a reproductive cycle, in perimenopause there are hormonal ups and downs, which create (or contribute to) the seemingly random and unpredictable physical and psychological manifestations we experience.
This stage can be as short as a few years, or longer than a decade.
Menopause marks the end of menstrual cycles.
“Officially”, menopause occurs when a woman hasn’t had a period for 12 months in a row. But there are different ways menopause can occur:
“Natural” menopause: When estrogen, progesterone, and other gonadal hormones (our reproductive / sex hormones) decline on their own as a result of aging.
Premature (or early) menopause: When menopause occurs before the age of 40. Sometimes, we don’t know why this happens. Other times, there are known risk factors, including medical conditions like diabetes or hypothyroidism; certain medications; pituitary damage from brain trauma (e.g. a history of concussions); smoking; or genetic inheritance.
Artificial menopause: When menopause occurs when ovaries are removed or damaged (for example, by some types of cancer treatments). Because of the sudden drop in hormones, menopause symptoms begin abruptly and may be more severe than other versions of menopause.
In women without a uterus, menopause can be identified by very high levels of follicle-stimulating hormone (FSH), which shows that the brain is telling the ovaries to increase production, but the ovaries aren’t listening. High FSH occurs in all women during menopause.
Postmenopause describes the phase after menopause.
At this point, hormonal fluctuations have leveled out, gonadal hormone production has shut down, and levels of most reproductive hormones are now relatively low.
Hormonal changes drive these shifts.
But what does “hormonal change” even mean? And what do hormones do?
Hormones signal our body to do stuff.
Most hormones act widely throughout the body. So, our reproductive hormones don’t just affect our reproductive organs.
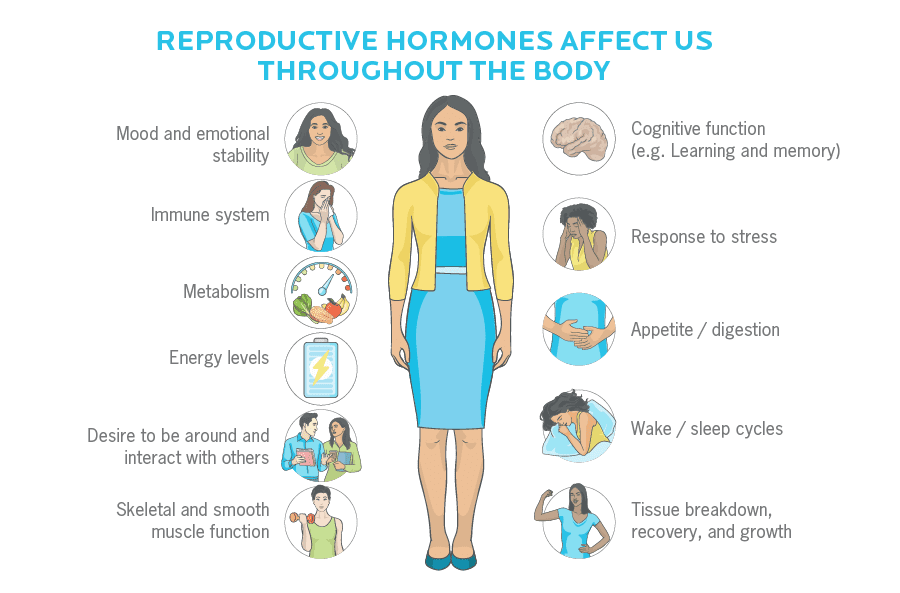
When hormones change, we change too.
Hormones are complex, and everyone’s are a little different.
When we say “hormones”, what we’re really describing are dozens, if not hundreds, of bioactive chemical compounds that make up complex signalling networks in our bodies.
For instance, “estrogen” is more accurately “estrogens”:
- estrone (E1);
- estradiol (E2);
- estriol (E3); and
- several other molecules that have estrogenic activity (in other words, that act somewhat like estrogen does).
And along with our gonadal hormones, we also have many other key hormonal systems, such as:
- thyroid hormones;
- neurotransmitters (e.g. serotonin, dopamine, and oxytocin);
- gastrointestinal hormones such as insulin;
- adipose (fat) tissue hormones such as leptin.
Then, there are other cell signalling molecules, known as cytokines, which play with hormones.
All of these molecules interact with each other, and all are governed by our genetic and epigenetic expression, as well as various other factors.
Each one of us has a unique, ever-changing “hormone fingerprint”.
This means that menopause is not as simple as flipping an estrogen on-off switch, and everyone’s hormones are affected by their unique genetics.
That’s part of why menopause is such a different experience from person to person.
Hormones change for many reasons.
While all of the interactions of our reproductive systems are far too complex to predict, one thing is clear:
The hormonal phenomena and experience of perimenopause, menopause, and postmenopause are all strongly affected by other factors.
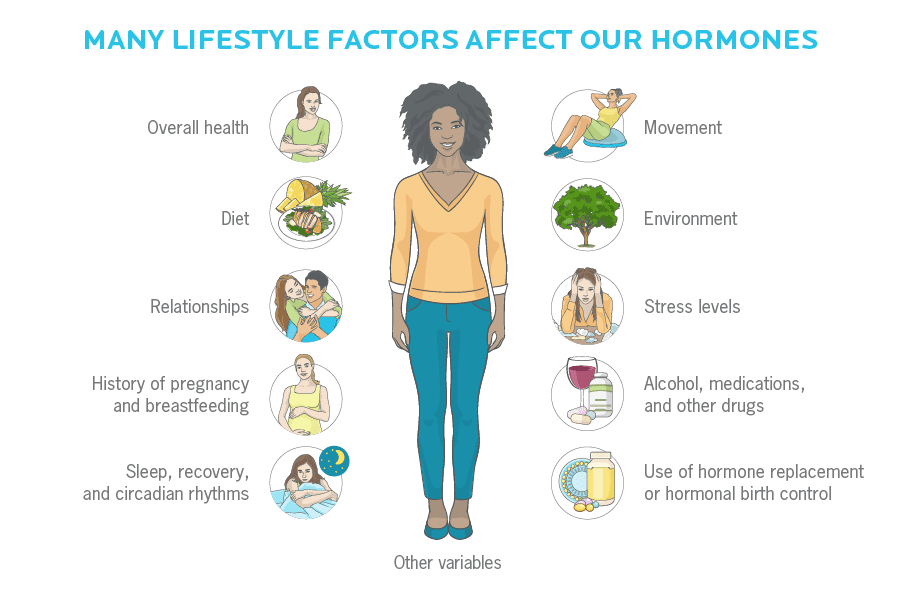
Some things, like what we choose to eat, how we work out, or what meaning we make from our experiences, we can control. Others, like our genes, or how often our bedmate disrupts our sleep with their snoring, we can’t.
Here are the changes you may notice during menopause, plus what can help.
Symptoms of hormonal changes might show up consistently, intermittently, or rarely.
They might be intense or barely noticeable.
But remember:
- Each woman’s experience is unique.
- These changes aren’t “just” biological. They’re also closely linked to our thoughts, feelings, relationships, and environments.
- Many of these symptoms aren’t inevitable. Your environment and behaviors can, to some degree, affect the outcome.
There’s only one given: Endogenous (self-generated) sex hormone production will decline. Everything else is like that randomly appearing repair person: Don’t plan your day around it.
Bladder
Decreased estrogen can lead to a reduced ability to control the urinary tract. You may have to pee more often, get more bladder infections, and have trouble controlling your bladder as pelvic muscles weaken due to aging.
What can help:
- Exercises from a pelvic physiotherapist to rehabilitate and prevent stress incontinence (when physical stress — such as coughing, sneezing, or laughing — causes an involuntary loss of urine)
- A vaginal pessary (a removable device that you insert into the vagina that supports pelvic organs) recommended by your doctor, especially if you have uterine prolapse
- Staying hydrated, peeing after sex, and supplementing a simple, safe carbohydrate known as D-mannose dramatically reduces bladder infections
Body composition
Changing hormones also lead to changing shape.
Lean mass (muscle, bone, and connective tissues) goes down while body fat goes up, a phenomenon known as sarcopenia.
You might notice more fat around your middle and lower belly in particular.
What can help:
- Quality nutrition
- Regular exercise
- Hormone replacement therapy (which may decrease abdominal fat), if you choose to take it
About 15 to 25 percent of women find their menopause symptoms so severe that they need hormone replacement therapy (HRT), which usually involves some combination of prescription bioidentical (i.e. just like the molecules our bodies make) estrogen and progestogen pills, patches, creams, or injections.
Most menopause symptoms are triggered by a sudden drop of estrogen, rather than a lack of estrogen overall. HRT that includes estrogen may stabilize levels and alleviate symptoms of menopause.
Because HRT has some risks, choosing it as a therapy depends on a woman’s personal medical history, family medical history, age, and symptom severity. All of these factors should be discussed with a doctor.
Benefits of HRT include relief from symptoms like hot flashes, vaginal dryness and thinning, sleep disruption, and low libido. Increased estrogen also means a better chance of preventing postmenopausal osteoporosis and fractures.
Unfortunately, HRT may also increase the risk of cancer (especially breast cancer) as well as heart attack, stroke, and blood clots.
For now, both the medical community and the research support short-term use of HRT to treat moderate to severe symptoms in healthy women in early menopause. Short-term use of low-dose HRT in healthy women (who have no specific contraindications) does not show increased risk of coronary heart disease, clotting disease, or specific cancers.
As an alternative to HRT, regular exercise, calcium, and vitamin D also play protective roles in maintaining healthy bones.
Anti-inflammatory and antioxidant-rich foods such as fresh fruits and vegetables, and phytoestrogenic foods such as soy and omega-3 rich flaxseeds may help to alleviate the severity and frequency of hot flashes.
If you’re suffering from moderate to severe symptoms of perimenopause / menopause, discuss your options with your doctor or another trusted healthcare practitioner.
Brain function
Hormones can affect thinking, reasoning, perception, and memory. Many women notice “brain fog” or trouble remembering things with declining hormones.
What can help:
- Quality nutrition
- Managing stress
- Regular exercise (as exercise boosts brain function due to the effects of increased blood flow as well as elevated brain chemicals such as BDNF, which is involved in learning and memory)
- Getting enough sleep, if possible
Breast health
Breasts and nipples may become more lumpy and tender. You’re also now at a higher risk for breast cancer.
What can help:
- Quality nutrition
- Regular exercise
- Limiting alcohol consumption
- Limiting or discontinuing use of medications that contribute to breast tenderness, like hormone replacement therapy, hormonal birth control, and some types of antidepressants
Digestion and bowel function
We tend to make less of our digestive enzymes and stomach acid as we age. Our smooth muscle tissue and intestinal absorption isn’t as peppy as it used to be.
This means you may notice changes in appetite, digestion, and bowel function. Heartburn, gas, and constipation might become your dinner companions more and more.
You may notice new food intolerances and sensitivities. Red wine?! Avocado? Really??
What can help:
Disease risk
“Female hormones” typically lower our risk of chronic diseases, such as cardiovascular disease, cancer, and so on… at least, until they run out. Then, our risk of these chronic diseases becomes greater.
What can help:
- Quality nutrition
- Regular exercise
- Managing stress
- Hormone replacement therapy, depending on the type of hormones prescribed, what age you start, and other risk factors (HRT also may increase risk for other diseases)
Dizziness / vertigo
Dizziness can occur with changes in how your brain regulates blood pressure (see temperature regulation below).
Women may also notice cyclical benign paroxysmal positional vertigo (BPPV), a sensation of spinning or dizziness occurring when their head is in particular positions, or when lying down or turning over. While we don’t completely know why this happens, researchers think that declining estrogen weakens the protein matrix that makes up our vestibular (balance) system in our inner ear.
Dizziness can also be related to migraines.
What can help:
- Staying hydrated, as changes in hydration and sodium levels can affect dizziness and vertigo
- Discontinuing medications that contribute to dizziness and vertigo, such as sedatives
- Balance training
- Two simple exercises: the Epley maneuver, or the half-somersault maneuver designed by Dr. Carol Foster, who created it to treat her own vertigo
Hair
Hair may grow more in some places (like on the face), and less in others (scalp, lower legs, armpits, pubic region).
What the heck, biology?
What can help:
- Hormone replacement therapy (for hair loss)
- Unwanted hair is one challenge our society has solved pretty well. To the wax mobile!
Menstrual cycles
Obviously, menstrual cycles change. They may become more or less frequent, heavier or lighter, more or less painful. Sometimes, they may be astonishingly heavy, like “Hahaha, Super Plus tampon, I will take you DOWN” heavy.
While you can’t do much to affect menstrual frequency or duration, nor the eventual end of menstruation, you can often improve related symptoms, like cramps.
What can help:
Migraines / headaches
Migraines can be stunningly painful or completely painless. For example, with “aura migraines” or ocular migraines, you might see the characteristic sparkling or flashing visuals of a regular migraine without pain. These are typically harmless and resolve in about 20-30 minutes. Other times, a migraine can make you want to submit yourself to a guillotine.
Hormonal fluctuations during perimenopause and menopause can exacerbate headaches and migraines, although these seem to settle after menopause.
What can help:
- Quality nutrition
- Keeping a “trigger diary”, which may help you notice that certain things (such as what you eat or your stress levels) make a migraine more likely
- Hormone replacement therapy or hormonal birth control (for those in perimenopause) may also affect headaches / migraines
Mood and mental health
Mental health covers a wide range of feelings, experiences, and domains, but in general, you might notice:
- More depression, “blahs”, emotional flatness, trouble “getting motivated”
- A sense of overwhelm or “it’s all too much”
- Feeling more irritable or less able to deal with small hassles
- Feeling more anxious, worried, fearful, or risk-averse
- Feeling distracted and/or preoccupied, having racing thoughts
- Crying or other emotional outbursts that happen more often, more unexpectedly, and/or more intensely
- More mood swings, and/or stronger swings
- More intense emotions, positive or negative
- Everyone around you has suddenly turned into a jerk
These mood changes can be attributed to not just variation in hormone levels, but also all the other biopsychosocial shifts that happen during menopause.
For instance, you may have good reasons for those mood swings. Maybe it is all too much, and this is a signal to make some important changes in your life choices, relationships, workload, etc.
What can help:
- Managing stress
- Counseling and/or coaching
- A good social support network
- In consultation with your doctor, medication like antidepressants
Pain and inflammation
Progesterone and estrogen are linked to pain and inflammation.
As sex hormones decline, you may notice changes in muscle pain, arthritis, other types of joint pain, pelvic pain, or flare-ups of other chronic pain concerns.
What can help:
- Quality nutrition
- Regular exercise
- Limiting alcohol consumption
- Managing stress
- Prioritizing sleep and recovery
- Non-pharmaceutical pain treatments, such as acupuncture, that work by “distracting” nociceptors (pain nerves)
- Relaxation and mindfulness training, which has been shown to help with how we experience pain
Sexual function
As estrogen and progesterone decline, the vaginal and urethral epithelium (lining) thins and becomes less elastic. Additionally, lubrication decreases, so the vagina will be drier.
This means that penetration can cause burning, itching, and a feeling like sandpaper on a sunburn.
Libido fluctuates. You may feel more liberated and sexy at midlife — many women say they’re having the greatest sex of their life, because they’re so much more confident, experienced, and assertive.
Or, you may feel like you don’t want anyone touching you, and would give up sex for sleep or chocolate 100 percent of the time.
What can help:
- Managing stress
- Doctor-prescribed estrogen creams or lubricants that you can apply to the vaginal area in order to reduce chafing, dryness, and tissue thinning
- For a non-hormonal option, one study showed that a vaginal gel containing hyaluronic acid (a natural compound involved in tissue repair and moisture regulation) was nearly as effective as estrogen cream at reducing symptoms of vaginal dryness
- Although vaginal tissue atrophies as a result of declining estrogen, the clitoris shows no such signs of stepping down from its position of pleasure glory. Just sayin’.
Skin
You may notice your skin getting drier or oilier as hormones shift. Perhaps you’re even getting some teenage-style acne.
Protein synthesis slows, so you’ll start to wrinkle, heal slower, and have less collagen. You’ll also likely lose fat from your face, and things will start to sag (because, gravity). You may notice changes in skin pigment.
What can help:
- Quality nutrition
- Prioritizing recovery and sleep
- Staying hydrated; not smoking; moderating sun and pollution exposure
Teeth
Your dentist might start making tsk-tsk noises about gum disease, receding gums, dry mouth, and so on.
What can help:
- Quality nutrition
- A good oral health routine (Make your dentist happy!)
- Not smoking
Temperature regulation
Hot flashes are one of the most puzzling and annoying experiences of menopause.
About 85 percent of North American women report having hot flashes during perimenopause and menopause, and 10-15 percent of them say these temperature changes are so severe that they interfere with daily life.
On average, hot flashes persist for 3-5 years.
Most women describe a hot flash as a feeling of extreme warmth, usually in their upper body and face and lasting a few minutes. Night sweats, as the name implies, are hot flashes that happen at night — you wake up flushed and sweaty, often enough to soak through clothes or bed sheets.
Hot flashes and night sweats seem to be triggered by a sudden dips in estrogen levels, rather than declining estrogen overall.
Body temperature can also be affected by changes in the brain’s vasomotor center, which regulates your blood vessels, making them tighter (vasoconstriction) or more open (vasodilation). However, we still don’t know exactly how the change in estrogen levels affects the vasomotor center.
What can help:
- Quality nutrition
- Paced breathing exercises. Try it: Breathe in from the belly while slowly counting to 5. Then, release the breath while slowly counting to 5. Practice this every day for 10-15 minutes. When a hot flash hits, start paced breathing and continue it for 5 minutes. Bonus: Paced breathing may also help lower blood pressure, decrease anxiety, and promote relaxation.
Aging is part of life.
In biology, cells senesce — they naturally deteriorate and decline with age.
We can speed this process up, or slow it down, but (for now) we haven’t quite figured out how to stop it altogether.
One thing we do know?
The changes that come with aging — like menopause — are not just in a physiological vacuum.
In other words, the changes we experience during menopause are not just tied to what’s going on with our bodies. Our mindset, the people we spend time with, and the life changes we’re experiencing matter, too.
Life changes are biospsychosocial.
When we experience life changes, they’re due to a complex interaction of the biological, the psychological, and the social dimensions of our lives.
For instance, many of our female nutrition coaching clients are tireless workers and caregivers — whether that’s at work, home, school, or out in the world.
The women we speak to are trying get their kids to school AND write their thesis AND deadlift with proper form AND visit Aunt Ruby who’s recovering from her hip replacement AND remember to vote AND stir the pasta sauce that’s about to bubble over on the stove.
So, if a woman feels fatigue or mood swings — two symptoms of perimenopause or menopause — what’s the “real” reason?
Hormones?
Stress?
Other people?
Not chanting enough positive affirmations?
The answer may be “several of the above” (but probably not the last one).
Often, menopause coincides with other life changes.
These can include:
- The “empty nest” phase. If you have kids, they usually move out (eventually). Suddenly, your focus shifts from offspring-rearing to… what?
- Relationship adjustments. If you have a partner, they’re getting older too. Or maybe you’re grappling with divorce, coming out, or starting to date again.
- Aging parents. If you have parents (or older relatives) who are alive, they may be dealing with health problems or need more attention.
- Work burnout. You gave at the office… and gave, and gave. What was an inspiring career path at 30 now feels like a joyless death march at 50.
- A desire for change. You may not have the feverish energy that you used to, but you may find yourself thinking about beginnings: new careers*, new relationships, new places to live.
*Fun fact: Nearly 10 percent of our Precision Nutrition Certification students start a new career at midlife. In fact, one of the authors of this article, Pamela Ruhland, went back to university at 45, did her PN Certification at 48, and was then hired to be an in-house coach with PN on the eve of her 50th birthday!
All these shifts in identity, responsibility, and interest may feel a little disorienting.
But they also create openings for positive change.
Menopause is a great time to build new healthy habits — and maintain current ones.
Many women say middle age is a time of empowerment.
During this period of life, some things die (such as our simplistic youthful illusions, or any desire to wear a crop top).
But new things will grow — fresh identities, opportunities, possibilities.
Women say they feel:
- More authentic: They care less about what others think and feel more free to be themselves.
- More courageous: They’ve been through it all, so why not?
- Less willing to tolerate BS: They’ve put up with crap long enough. They reclaim their time.
Experiences, even difficult ones, bring insight, wisdom, and resilience.
By midlife, we’ve built a nice set of life skills, and we’re looking to use them in new ways.
If you’re going through perimenopause or menopause, you probably won’t like all the changes you’re experiencing.
But remember that that bidirectional relationship between your hormones and the rest of your body that we described earlier?
Just as hormonal changes can affect your sleep, body composition, mental health, and more, your daily habits can impact how strongly you feel the impact of those hormonal shifts.
You’ve got power, lady.
6 lifestyle strategies that can help alleviate menopause symptoms.
Strategy #1: Prioritize quality nutrition.
At this point in life, you may be ready to say goodbye to 10-day cucumber cleanses, fad diets, and get-fit-quick plans. We say: Right on!
And here’s some very good news:
Good nutrition can ease or even alleviate much of the discomfort of midlife physical changes, plus it’ll help you maintain a healthy body composition.
Many of our clients find that through quality nutrition, they can manage their appetite and improve their digestion and bowel habits. (‘Cause no matter how old you are, a good poop is still terrific.)
Prioritizing good nutrition can also decrease disease risk, help manage symptoms of changing menstrual cycles, reduce inflammation (and inflammation-related pain), improve skin quality, and promote dental health.
How to do it:
Most of us are busy, rushed, and hovering over our keyboard as we eat our tuna salad. Slow down and pay attention. This will help you know when you’re truly physically hungry, and when you’ve eaten the amount your body needs.
It’ll also help to alleviate digestive upset like bloating and heartburn, which are really just your body’s way of avenging that spicy calzone you just ate in 17 seconds.
If good nutrition is a goal, consider:
- Carbohydrates: Eat 1-2 cupped handfuls of slow-digesting, high-fiber carbohydrates at most meals, unless you have a reason not to do so (e.g. an aggressive intervention to manage your blood sugar).
- Protein: Evidence suggests that our protein needs go up, not down, as we age. More protein means more lean mass and better bone density, especially if you’re also doing resistance training. Shoot for at least 1 palm-sized portion of protein at most meals. More protein can also help with skin quality as we age. Here’s more advice.
- Phytoestrogens: The research on phytoestrogens in food (such as soy) suggests that they may help with hot flashes… or they may not. In other words, it’s not entirely clear. Feel free to experiment with adding soy to your diet, especially more traditional versions like fresh edamame, miso, and tempeh. These are consumed in Japan, China, and other Southeast Asian countries, where women have much lower rates of hot flashes.
If you have a family history of breast cancer and/or the BRCA gene, check with your doctor before adding estrogenic foods.
- Hydration: Drink plenty of water and keep your salt intake moderate. This can help with water retention and breast tenderness, which can fluctuate over your cycle, as well as skin quality.
- Vitamin D: Some evidence suggests that vitamin D can lessen perimenopausal and menopausal symptoms. Get your D levels checked, and if they’re low, either book that tropical vacation you’ve always wanted (hey, it’s for medical reasons), or supplement. Vitamin D is also important for maintaining bone health.
- Caffeine: Notice whether caffeine in coffee, tea, energy drinks, dark chocolate or medications (such as painkillers) triggers or exacerbates any symptoms you have, such as breast tenderness or migraines. Experiment with reducing or avoiding caffeine to see if it’s worth the trade-off.
- Flaxseed: Flaxseeds are rich in plant compounds called lignans. With the help of intestinal bacteria, lignans can be converted to weak estrogens (enterodiol and enterolactone) which may help reduce menopausal symptoms.
- Omega-3 fatty acids: Omega-3 fatty acids (2-6 grams a day) may help with some symptoms, like hot flashes, depressive symptoms, and memory decline. There also may be added benefit to starting supplementation before the onset of perimenopause, although the research is unclear. Including high-quality fats in your diet may also help with skin changes.
- Iron: If you’ve stopped menstruating, you’ll need less iron (down to about 8 mg a day), unless you’re doing something else that increases iron needs, like Ultimate Fighting. (Pfff, after 30 odd years of monthly bloodshed, a nosebleed doesn’t even make you blink.)
- Calcium: For bone health, calcium needs increase during menopause to about 1200 mg a day, preferably from food sources such as quality dairy products; cooked dark leafy greens; bone-in canned salmon or sardines; or calcium-fortified foods.
- Magnesium: Magnesium is important for calcium metabolism and also helps preserve bone health. Supplemental magnesium (200 – 400 mg / day) may also help alleviate hormone-related cramps and migraines.
Strategy #2: Approach alcohol intake mindfully.
The image of middle-aged women who love wine has become a cultural cliché.
You’ve seen the t-shirts at those tacky souvenir shops. “Wine is for women what duct tape is for men: It fixes everything!” they read in bold pink letters.
But although a buttery Chardonnay goes nicely with fish, it doesn’t necessarily pair well with our bodies, especially as we age and our livers become less efficient at processing it.
Limiting alcohol consumption may help reduce inflammation, as well as your risk of breast cancer and other diseases.
How to do it:
Notice where, when, how, and with whom you drink. Are there certain triggers — like work functions, or your friend Marie — that always seem to end with you having a strong urge to dance on (or lie under) the table?
Notice what happens if you think about (or actually do) stop drinking for a week or two.
There’s no “right” amount to drink. You may choose to drink less for your health, or you may drink more because you genuinely enjoy it and want to prioritize pleasure.
Either way, drinking should always be a calm and conscious choice, rather than an obligation or compulsion.
Strategy #3: Commit to regular exercise that you truly enjoy.
Exercise (moving at moderate intensity 2-4 times per week for 30-60 minutes per session) seems to help with menopausal symptoms like cramps associated with changing menstrual cycles and inflammation, though it varies from woman to woman.
Women who have lower fitness levels going into exercise sessions may be less likely to see a benefit, which has made interpreting the impact of exercise more difficult.
Still, regular exercise is your best shot at having a healthy, strong, functional body composition. This means lots of protective lean mass (like strong muscles and bones) and less body fat (especially the more risky stuff around your internal organs, called visceral fat). It also means a lower risk of disease, including breast cancer.
How to do it:
You may have less time to exercise right now, which means you’ll have to get creative about squeezing in movement when you can.
Or maybe you have more time. Your 20-year-old son may still live at home but it’s time he does his own laundry… because you’re off to Zumba.
Here are some guidelines to consider for exercising during menopause:
- If you still love intense workouts, recognize that you’ll need more recovery. And have a good physiotherapist on speed dial.
- Whether it’s a full yoga routine or simply a 5-minute mobility warmup, make sure to include regular joint mobility / injury-prevention type movements to keep joints lubricated and flexible.
- Do some weight-bearing movements / resistance training at least 2-3 times a week. This tells your bones, muscles, and connective tissues that you need them to stay dense and strong.
- Start where you are. If you’re just picking up an exercise habit for the first time in midlife, start gently. In women who are sedentary, yoga may be a good activity to start with and has been shown to improve quality of life in menopausal women.
- Consider making it social. Many of us are more likely to stick with things if we have accountability, support, and community. Join a class or group, or find a workout buddy. Or get a dog. Their toilet is outside, so they’re always motivated for a walk.
- Keep cool. Your body is having a tough time regulating your temperature, so exercise in a cool place and drink cool fluids.
- Consult with a physiotherapist who specializes in pelvic rehab if you’re noticing you’re peeing during squats, jump rope, or other movements, or if you’re having pelvic pain under load.
- If you use a trainer / coach, make sure they understand how to train a body at midlife. They should be able to balance challenge with respect for any limitations you have.
- Have fun. That’s an order.
Strategy #4: Practice self-compassion, especially when it comes to your body.
When your sleep is disrupted by a hot flash that rivals the fires of Mount Vesuvius, or when you’re urging your hips into jeans that used to feel roomy and now feel like sausage casings, it’s understandable to feel angry and frustrated. Or even sad.
At midlife, you will put on more body fat. As ovarian production of estradiol (a type of estrogen) shuts down, our body relies on our adipose (fat) tissue (along with a few other types of tissue) to produce similar hormones.
We actually need that extra bump in our rump to keep us healthy as we age.
And it turns out, there’s a “sweet spot” for our body composition.
While having enough body fat will maintain hormonal health, too much body fat increases our risk of estrogen-dependent cancers (e.g. ovarian and breast cancer) as well as other metabolic diseases.
So, it’s important for your health to be conscious of your body composition, but it’s also key to make peace with your body as it is now.
How to do it:
Forget about the celebrities that somehow look 25 when they’re 55. They pay a team of surgeons, personal trainers, stylists, and magical wizards to keep them camera-ready.
Define what “fitness” and “health” mean for you.
Decide what you value, in terms of your physical self.
Maybe you value strength more than aesthetics, and maybe you don’t. (Although it does feel good to know you can open any pickle jar life throws at you.)
Your body will change. You will look different. Whatever you feel you’ve lost, mourn it.
Punch and cry snottily into your pillow. Burn an effigy. Do whatever you need to do to herald the end of the old and the beginning of now.
Then, consider what a sane, realistic, and achievable set of expectations and goals for yourself look like right now. (If you aren’t sure, check out The Cost of Getting Lean.)
Approach these goals with self-compassion rather than self-criticism.
Strategy #5: Prioritize and schedule recovery and sleep.
When things don’t go the way we want, most of us do more and push harder.
For example, if your waistline has changed despite being a regular exerciser and mindful eater, you may (understandably) think it makes sense to add more and higher intensity exercise, combined with less food on your plate.
Grrr, that should do it.
But it doesn’t.
While you may not think of exercise as a stressor, it is.
Exercise requires your body to work harder. And work = stress (even when it’s “good” stress.)
With every stressor you add on, you also need proportionate recovery from it.
Restricting food is also a stressor. Women who worry about limiting food intake to manage body weight tend to have higher levels of cortisol, a stress hormone, than women who don’t.
Add that to the sleep disruptions so common in menopause (between 40-60 percent of women going through menopause have poor sleep quality or insomnia), and your “stress bucket” is getting pretty full.
Lower estrogen levels also means your body has a decreased capacity to deal with stress. That bucket fills up quicker than it used to.
Even though many stressors are good for us (like exercise, learning, and change), they only make us stronger if we give ourselves the chance to recover from them.
Not getting enough recovery and sleep can also contribute to pain, inflammation, and age-related skin changes.
How do to it:
Check in with yourself. Are you exhausted? Are your workouts feeling like a heavy slog?
If so, try this radical idea: Take a week off from the gym. Focus on activities that are less intense and more pleasurable. Like taking your dog for a walk in the park, or paddling around in the pool.
When you go back to the gym, notice how you feel. Do you have more energy? Or a renewed sense of interest? Are your muscles feeling stronger or less achey?
Play around with exercise frequency and intensity. Try reducing the number of sessions a week or decreasing the intensity of a few sessions. Replace some higher intensity weight training or cardio sessions with lower intensity sessions like yoga or long walks.
Every month or so, schedule a “recovery week”. For that week, decrease exercise volume, or skip the gym altogether and just engage in gentler movement like stretching, foam rolling, tai chi, or quiet hikes in nature.
Sleep is also a key part of recovery. If you have difficulty sleeping, here are some things to try:
- See what you can do to reduce hot flashes, which can disrupt sleep.
- Practice good sleep hygiene.
- See a therapist who specializes in sleep. Cognitive behavioral therapy or hypnosis designed specifically for insomnia can be effective.
- Try exercise like yoga, weight training, or brisk walks, which can improve chronic insomnia in perimenopausal women.
- Experiment with natural remedies like valerian root, tart cherry juice, and isoflavones (from soy), which may improve sleep.
- Talk to your doctor. Certain prescription medications, such as hormone replacement therapy or low-dose SSRI’s can help.
- Get a massage. Because anything that makes you drool from bliss and relaxation is good.
- Many women even opt for a separate bedroom if they have a partner whose flailing and snoring is making their already-fragile sleep unworkable.
Strategy #6: Take steps to manage your stress.
You may find that, compared to your younger years, you just don’t care as much about what people think of you. This can be hugely stress-relieving.
But thanks to all the changes you’re going through, you may also be dealing with feelings you’re not used to, sometimes swinging wildly.
Unmanaged stress can have a negative impact on your sex life, brain function, pain and inflammation, and overall disease risk — not to mention your overall quality of life.
How to do it:
Coaching or counseling, mindfulness or relaxation practices, and other mental health strategies can dramatically improve your existing mental health or preserve the wellbeing you have. Mindfulness and relaxation practices can also help manage pain.
If the mood fluctuations or psychological distress are severe and causing problems with your daily-life function, consider consulting a mental health professional. For instance:
- You might consider getting coaching or counseling.
- You might consider speaking to your doctor or psychiatrist about antidepressant or anti-anxiety medication.
- Also discuss these feelings with your doctor or psychiatrist if you’re on hormone replacement therapy.
Your mental state also affects your sexuality.
Setting aside time for yourself, learning to have healthy relationships, and practicing good “intimacy habits” can also help you feel juicy and sexy. Consider looking at other factors in your life and relationships to see if you can bring some calm, joy, and ooh-la-la back.
Speaking of relationships, consider which ones are serving you right now. Are there any relationships that you need to let go of, or adjust so that they feel healthier?
At this point in life, it’s helpful to be willing to let go of (and grieve, if necessary) old patterns and identities. Maybe your primary identity used to be “Mom”, and that doesn’t fit as well anymore now that your kids have moved out and you’re itching for adventure.
Be open to stepping into new versions of yourself and new ways of relating.
Menopause can be a gift… it kinda means you “made it”.
Many of our prehistoric ancestresses didn’t survive past the age of 40.
In some ways, making it past the childbearing years and into the “wise elder” years is a luxury.
While men can theoretically reproduce until they die (um, not that we’re recommending that), menopause signals the end of a woman’s ability to have children.
It’s kinda like nature is telling us, “Nah, it’s time for you to do you now. The rest of your life is for you.”
Hm. Why thank you, Mother Nature.
What will you do with that gift, that wide open space of possibility?
What to do next:
Some tips from Precision Nutrition
Don’t worry about fixing everything… or anything.
Remember, you aren’t broken.
Menopause is a normal, inevitable, adaptive stage of womanhood.
You’re totally allowed to sink into the hammock of biology and let your body work this out without intervention.
If you are considering positive changes to feel better, pick one small thing at a time.
Practice that change consistently, then add on more if / when you feel ready.
Keep a journal of your experience.
Write your own Owner’s Manual. You’re the expert on you.
If you have a symptom that’s especially vexing, consider tracking it and notice any patterns. For example, you may notice that when you have coffee, your cramps are worse. Or every time you watch CNN, you get a hot flash.
Get to know the natural rhythms of your body over time by gently and non-judgmentally noticing and recording what comes up.
Use your emotions as tools (instead of being possessed by them).
Just like puberty, menopause is a time of intense hormonal flux, and corresponding emotional and physical changes.
But unlike your 15-year-old self, you are now a grown-up ladyperson, and you can choose to make use of the feelings that come up, instead of being owned by them.
When sadness comes up, you might look at what you need to grieve or let go of. When anger comes up, you might look at what needs to be protected or spoken up for. When fear comes up, you might look at what needs to be reassured or supported.
Use your emotions as tools to learn more about yourself, and to create a life that feels good for you.
Talk to other women.
Whether it’s a coach, a wise mentor, your mom, a friend, or that lady at the gym who just seems friendly and healthy, find and talk to older women about their experiences.
Not only will this give you practical advice (“Always dress in layers; never wear a pleather unitard”), it will also give you a feeling of support, normalcy, and sisterhood.
Several Precision Nutrition coaches have personal experience with perimenopause / menopause, or at least have coached hundreds of women through it.
Distribute your “craps given” wisely.
Perimenopause and menopause, with all its changes, may feel a little overwhelming for some.
Which is why you’re allowed to take some things off your plate.
Maybe you don’t give a crap anymore about “always being polite”.
Maybe you don’t give a crap anymore about fitting into a size X dress.
Maybe you don’t give a crap anymore about achieving “eternally youthful skin”.
You’re allowed to not care about whatever you don’t want to care about anymore.
Leave your caring for stuff you really care about.
Assemble your support team.
Think of the kind of support you need to be your best self at this stage of life.
You’ll probably want some loving friends or family members to talk to or reassure you.
A good family doctor or OBGYN you feel comfortable discussing all the gory bits helps too.
Add on whatever else you need, such as:
- A physiotherapist to help your pelvic muscles perform.
- A trainer to help you move safely and joyfully. (Maybe a boxing coach who can help you channel that pent-up rage healthily.)
- A coach or therapist to talk through difficult feelings.
- A naturopath, nutritionist, or dietician to help you figure out what foods will support your health.
- A “menopause mentor” who will remind you that you’re not going crazy.
- And so on.
Gather your posse, and conquer.
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We'll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)



Share